Addiction and Pancreatitis: A Comprehensive Study

Pancreatitis is a condition characterized by inflammation of the pancreas, a gland located behind the stomach. The pancreas is a vital part of the body as it plays a key role in digestion and blood sugar regulation by producing enzymes and hormones, including insulin.
Addiction is a complex, chronic condition characterized by compulsive drug-seeking and use despite harmful consequences. According to a 2017 World Health Organization report “ Drugs (psychoactive)”, 5.5% of the world population, or 270 million people, aged 15 to 64 years used psychoactive substances the previous year. One such consequence is pancreatitis, an inflammatory disease of the pancreas that leads to severe complications and even death if left untreated.
Causes and risk factors of pancreatitis related to addiction include alcohol abuse, smoking, genetic predisposition, dietary factors, and co-existing conditions.
Symptoms of pancreatitis linked to addiction include severe, persistent, abdominal pain radiating towards the back that worsens after eating. It also presents with nausea, vomiting, and fever.
Treatment approaches for addiction and pancreatitis are medical management, psychotherapy, medication-assisted treatment, social support, and lifestyle modifications.
What is Pancreatitis?
Pancreatitis is a condition characterized by inflammation of the pancreas, a gland located behind the stomach. The pancreas plays a crucial role in digestion and blood sugar regulation by producing enzymes and hormones, including insulin. Substances such as alcohol cause the pancreas to excrete excess digestive enzymes, resulting in inflammation. When the pancreas becomes inflamed, it leads to abdominal pain, nausea, vomiting, and other symptoms.
There are two main types of pancreatitis: acute and chronic. Acute pancreatitis typically occurs suddenly and lasts for a short period, while chronic pancreatitis is a long-term condition characterized by persistent inflammation and damage to the pancreas. Chronic pancreatitis results in irreversible changes to the pancreas, leading to complications such as pancreatic insufficiency, diabetes, and pancreatic cancer.
Did you know most health insurance plans cover substance use disorder treatment? Check your coverage online now.
What Are The Causes and Risk Factors of Addiction-Related Pancreatitis?
Causes and risk factors of addiction related to addiction include alcohol abuse, smoking, genetic predisposition, dietary factors, and co-existing conditions.
The relationship between addiction and pancreatitis involves biological, behavioral, and environmental factors. One of the primary mechanisms linking addiction to pancreatitis is the direct toxic effect of substances on the pancreas. Alcohol, for example, causes pancreatic injury by triggering pancreatic enzyme activation and oxidative stress, leading to inflammation and tissue damage.

Alcohol abuse
Alcohol abuse is one of the leading causes of pancreatitis, particularly chronic pancreatitis in the US. According to a 2023 study by Klochkov A., et al, “Alcoholic Pancreatitis”, published in StatPearls, heavy and prolonged alcohol consumption leads to pancreatic damage and inflammation, increasing the risk of developing pancreatitis. Chronic alcohol consumption is known to disrupt pancreatic function and impair the secretion of digestive enzymes and hormones, contributing to the development of pancreatitis.
Smoking
Smoking is another significant cause and risk factor for pancreatitis, often working synergistically with alcohol to exacerbate the risk of pancreatitis. According to a 2015 study, “Impact of Smoking on the Risk of Pancreatitis: A Systematic Review and Meta-Analysis”, published in the PLOS One journal, cigarette smoking increases the risk of developing pancreatic problems including cancer. Smokers with heavy alcohol consumption habits have a higher risk of developing chronic pancreatitis compared to non-smokers.
Contact us today to schedule an initial assessment or to learn more about our services. Whether you are seeking intensive outpatient care or simply need guidance on your drug addiction journey, we are here to help.
Illicit drugs
Cocaine use induces vasoconstriction and decreases pancreatic blood flow, leading to ischemia and tissue damage. Opioids, on the other hand, cause sphincter of Oddi dysfunction, a condition characterized by abnormal contraction of the muscle that controls the flow of bile and pancreatic juices into the small intestine, potentially triggering pancreatitis.
Poor dietary choices
Dietary habits play a role in the development of pancreatitis. According to a 2018 study by Dugum, M., et al, “Association of Dietary Habits with Severity of Acute Pancreatitis”, published in the Current Developments in Nutrition journal, a meat-intensive diet is associated with pancreatitis. In addition, a high-fat diet aggravates the effects of alcohol on the pancreas. Malnutrition, commonly seen in chronic alcoholics, also predisposes individuals to pancreatitis by weakening the body’s defenses against inflammation and infection.
Symptoms of Addiction-Related Pancreatitis
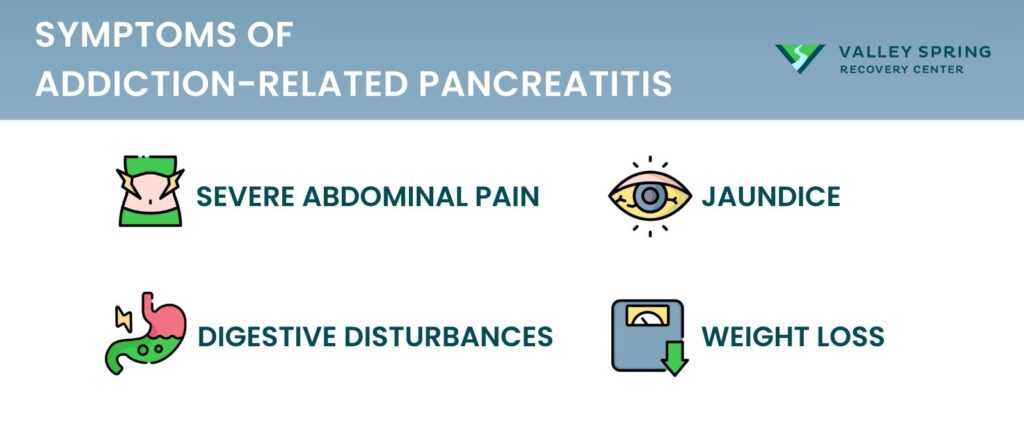
Addiction-related pancreatitis presents with severe abdominal pain radiating toward the back, nausea, fever, weight loss, and oily, foul-smelling stool. According to the article “Pancreatitis”, from the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), symptoms of pancreatitis include:
- Severe abdominal pain: Pancreatitis caused by substance abuse manifests as severe abdominal pain, which usually radiates to the back. The pain gets worse after eating and persists for hours or days. Nausea, vomiting, and fever usually accompany the pain.
- Digestive disturbances: Pancreatitis causes digestive disturbances, leading to oily, foul-smelling stools (steatorrhea).
- Jaundice: Jaundice, characterized by yellowing of the skin and eyes, may occur if the bile duct becomes blocked by inflammation.
- Weight Loss: Due to malabsorption and decreased appetite, significant weight loss is common in chronic pancreatitis.
Additionally, substance-related pancreatitis worsens existing conditions such as diabetes mellitus due to pancreatic damage affecting insulin production. In such circumstances, patients experience increased thirst, frequent urination, and unexplained fatigue.
Rediscover Life at Valley Spring Recovery Center
Get the compassionate support you deserve. We're here to help you reclaim joy, wellness, and a brighter future.
Verify Benefits
What Are The Treatment Strategies For Addiction-Related Pancreatitis?
Treatment for pancreatitis linked to substance abuse includes medical management, psychotherapy, medication-assisted treatment, social support, and lifestyle changes.
Medical Management
Initially, the focus is on stabilizing the patient’s condition. According to a 1997 study by Apte, M. V., et al, “Alcohol-Related Pancreatic Damage: Mechanisms and Treatment”, published in the Alcohol Health and Research World journal, medical interventions include bed rest, fasting, administration of intravenous fluids, and enzyme inhibitors to reduce the corrosive effects of pancreatic digestive enzymes.
Pancreatitis Treatment
According to a 2017 study by Drewes, A.M., et al, “Consensus Guidelines For Chronic Pancreatitis. Guidelines For The Understanding And Management Of Pain In Chronic Pancreatitis”, once the patient has been stabilized, physicians embark on treatment for pancreatitis involves strict dietary restrictions, with patients initially fasting to rest the pancreas and then gradually reintroducing clear liquids and eventually solid foods. Pain management is an important part of treating pancreatitis. This is achieved using analgesics and in some instances antibiotics to prevent infections.
Are you covered for treatment?
Valley Spring Recovery Center is an approved provider for Blue Cross Blue Shield and Cigna, while also accepting many other major insurance carriers.
Check Coverage Now!Addressing Addiction
To treat pancreatitis caused by substance abuse effectively, it is important to address addiction. This often involves a multi-disciplinary approach, including medical professionals, therapists, and addiction specialists. The 2017 study by Drewes, notes that treating alcohol-related pancreatitis requires the patient to abstain from alcohol. Normally, this includes detoxification, where patients undergo supervised withdrawal to safely rid the body of the addictive substance.
- Therapy and Counseling: Cognitive-behavioral therapy (CBT), motivational interviewing, and group therapy are commonly used to help patients understand the root causes of their addiction, develop coping mechanisms, and prevent relapse. Family therapy is also beneficial in addressing familial dynamics that contribute to the addiction.
- Medication-Assisted Treatment (MAT): In cases of opioid or alcohol addiction, MAT is prescribed to help manage withdrawal symptoms and cravings. According to the article” Medications for Substance Use Disorders”, from the Substance Abuse and Mental Health Services Administration (SAMHSA), medications like naltrexone, buprenorphine, or methadone are highly effective when used in conjunction with psychotherapy.
- Support Groups and Aftercare: Long-term recovery often necessitates ongoing support. Support groups such as Alcoholics Anonymous (AA) or Narcotics Anonymous (NA) provide a sense of community and accountability. Aftercare programs offer continued therapy and support to help individuals navigate challenges and sustain their recovery to avoid relapse.
- Lifestyle Changes: Adopting a healthier lifestyle, including regular exercise, adequate sleep, and stress management techniques helps in rehabilitating the addict and reducing the risk of pancreatitis recurrence.
- Monitoring and Follow-up: Regular medical check-ups and monitoring of pancreatic function are essential to track progress, manage any complications, and adjust treatment as needed.
Is Pancreatitis Always Caused by Drug Use?
No, there are other causes and risk factors of pancreatitis except substance abuse.
According to a 2020 study by Ágnes M., published in the Gastroenterology journal, drug-induced acute pancreatitis ((DIAP) accounts for 5 percent of all pancreatitis cases. In most cases, pancreatic symptoms may appear mild to moderate but still pose life-threatening risks.
Is Drug-Induced Acute Pancreatitis Reversible?
Drug-induced effects are reversible if the drug is discontinued which allows the body to metabolize and eliminate it. According to a 2017 study by Rebecca A. B., et al, “ Pancreas”, drug-induced acute pancreatitis is reversible as long as the offending substance is removed.
Did you know most health insurance plans cover substance use disorder treatment? Check your coverage online now.
Can Substance-Induced Pancreatitis Be Prevented?
It is possible to reduce the chances of developing pancreatitis by making healthy lifestyle choices. According to the article “Acute Pancreatitis Prevention”, from the National Health Service (NHS), cutting back on alcohol or drinking moderately reduces the chances of developing pancreatitis.
How Long Does Pancreatitis Take To Heal?
There is no definite time to heal from pancreatitis as this depends on factors such as the extent of the damage done and your general health. But on average, you should start feeling better in about 10 days unless you have other co-occurring conditions.
Can Drug-Induced Pancreatitis Go Away Without Medication?
Acute pancreatitis normally goes away on its own when the offending substance is discontinued. However, some people develop complications that need medical attention, so you should not manage pancreatitis at home. Chronic pancreatitis needs medical intervention.
Share This Post















