Addiction treatment is a specialized form of healthcare aimed at helping individuals overcome the compulsive and detrimental use of drugs or behaviors that lead to drug abuse. Treatment is an essential intervention that seeks to restore balance in various aspects of a person’s life that have been disrupted by addiction to substances. There are specific criteria and assessments used to determine the most effective treatment plan for an individual abusing substances.
Indicators that suggest the necessity for specialized addiction treatment include withdrawal symptoms, increasing dependency on the substance or behavior, and negative repercussions in both personal and professional spheres. These symptoms often guide the selection of treatment modalities, which can range from detoxification and medication-assisted treatment to cognitive-behavioral therapy and support groups.
There are multiple different types of addiction treatment philosophies, and the best treatment plan can be determined based on the underlying causes that lead to the need for addiction treatment. Causes and symptoms that require addiction treatment can be diverse, including biological factors, emotional triggers, and mental health conditions. These root causes often perpetuate the cycle of addiction, making targeted treatment in a specialized setting crucial for long-term recovery. Ignoring these factors can result in a host of health complications and strained interpersonal relationships, similar to those seen in untreated addictions.
A drug rehab center is a place where addiction treatment is administered that can lead to a myriad of positive outcomes such as improved mental health, social reintegration, enhanced physical well-being, and increased self-esteem. These centers also focus on equipping individuals with the skills needed for better performance in their work or educational pursuits, among other life improvements.
What Is Addiction Treatment?

Addiction treatment is a set of structured interventions that manage and mitigate addiction to drugs and related behavioral and mental health issues. Addiction treatment is a broad term that can be used to describe types of treatment or therapeutic interventions, which aid in the development of coping skills that support abstinence from substance use and promote a holistic recovery. Addiction treatment methodologies or types of treatment are diverse—ranging from holistic and evidence-based approaches to experiential therapies. Different treatment approaches can address some or all of the complex symptoms someone afflicted with substance use disorder is experiencing.
It’s important to understand “treatment” as a multifaceted term with different delivery methods and can occur in various environments. Addiction treatment occurs predominantly in drug rehab centers, which can be facilities, outpatient clinics, or performed virtually through telehealth programs. Addiction treatment also occurs outside of a rehab center on an individual basis with a therapist or psychiatrist or through peer recovery programs like alcoholics anonymous.
Thus, the term “treatment” in drug addiction care serves as an umbrella that covers an array of different methodologies that can be used at varying degrees of intensity and occur within the continuum of care defined by the level of treatment intensity where a doctor, psychiatrist, addictionologist, clinician or therapist provide treatment. These levels should be thought of not as discrete levels of care but rather as points in a continuum of treatment services according to Mee-Lee and Shulman’s NCBI study in 2003. Treatment can and should cater to the individual needs of each patient to address their symptoms and human experience. It seamlessly blends medical, psychological, and lifestyle perspectives, ensuring a comprehensive approach that is aligned with the multifaceted and complex nature of addiction.
What is the goal of addiction treatment?

The goal of addiction treatment is multifaceted, aiming not only to achieve and maintain abstinence from substances but also to address the broader spectrum of recovery needs. For many individuals, the primary objective is complete sobriety, which forms the foundation of a sustainable recovery journey. However, recognizing that total abstinence may not be the goal for everyone, modern treatments also focus on reduction-based goals. This approach allows individuals, such as alcohol users, to reduce their intake to less harmful levels.
In addition to these goals, addiction treatment emphasizes relapse prevention, which involves developing strategies to identify triggers, manage cravings, and cope with high-risk situations, thereby enhancing resilience and helping individuals avoid substance use during challenging times. Treatment also addresses the physical and mental health consequences of substance abuse, setting goals to improve fitness, correct nutritional deficiencies, establish healthy sleep patterns, and manage co-occurring mental health conditions through therapy and counseling.
Furthermore, recovery is viewed as an opportunity for personal growth and transformation. Goals in this area include improving self-esteem, enhancing communication skills, building healthy relationships, and engaging in activities that provide a sense of purpose and fulfillment. Building a strong social support network is also crucial, involving participation in support groups, therapy with family members, and fostering connections with sober peers. Ultimately, treatment goals for substance use disorders should be individualized to fit each person’s specific needs and circumstances, ensuring a comprehensive approach to recovery.
Goals for treatment vary based on the individual but are listed below in a general way.
- To Improve Quality of Life
- To Reduce Harm
- To Achieve Abstinence
- To Foster Behavioral Changes
- To Facilitate Community Support
- To Address Psychosocial Problems
- To Develop a Positive Support Network
- To Enhance Problem-Solving and Coping Skills
The goals for each level of addiction treatment, types of treatment, and specialized treatment programs differ in their scope and focus based on factors such as treatment population, program comprehensiveness, and philosophical underpinnings, they generally align on a set of core objectives. These objectives serve as guideposts, enabling healthcare providers and clients to navigate the complex pathway to recovery.
How to Determine the Right Type of Addiction Treatment?
Choosing the right type of addiction treatment is a critical decision that can significantly impact your recovery journey. Various diagnostic tools and personal considerations come into play when making this choice.
DSM-5 Criteria: The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), is a widely used clinical tool for diagnosing various mental health conditions, including addiction. The DSM-5 provides a set of criteria that healthcare providers use to assess the severity and type of addiction. These criteria can include patterns of use, withdrawal symptoms, unsuccessful attempts to quit, and the impact of addiction on daily life. Based on this assessment, professionals can recommend the most appropriate form of treatment, whether it’s inpatient rehab, outpatient therapy, medication-assisted treatment, or a combination thereof.
Human Approach – Personal Comfort and Needs: While clinical diagnostics are invaluable, they are not the sole determinants in choosing the right treatment. Your comfort level with the proposed treatment options is equally crucial. Some people prefer a more holistic approach that incorporates alternative therapies like yoga, meditation, or acupuncture. Others feel more comfortable in a group therapy setting, sharing experiences and coping strategies with peers. Financial considerations, such as insurance coverage and out-of-pocket expenses, can also influence your decision.
Balancing Clinical and Personal Factors: The most effective approach to determining the right type of addiction treatment often involves a balance between clinical diagnostic methods and personal preferences. For instance, healthcare providers use DSM-5 criteria to recommend inpatient rehab, but if you have work or family commitments that make this option unfeasible, outpatient therapy might be a more practical choice. Open communication with your healthcare provider about your personal needs and constraints is essential for tailoring a treatment plan that you’re comfortable with and that also meets clinical recommendations.
What Are The Different Types Of Evidence-Based Addiction Treatments?
In the realm of addiction treatment, evidence-based therapies are approaches that have been rigorously tested in controlled conditions and validated through peer-reviewed research. These methods are considered the gold standard for addiction treatment because they are rooted in scientific evidence, ensuring their efficacy. Here are some of the main evidence-based therapies:
Medication-Assisted Treatment (MAT):

Medication-assisted treatment (MAT) is a comprehensive approach to the treatment of substance use disorders that combines the use of FDA-approved medications with counseling and behavioral therapies. MAT is designed to treat the whole patient, addressing the medical, psychological, and social aspects of addiction.
MAT works by using medications to stabilize brain chemistry, block the euphoric effects of alcohol and drugs, relieve physiological cravings, and normalize body functions without the negative effects of the abused substances. The medications used in MAT are tailored to specific types of substance dependencies:
- Opioids: Medications such as methadone, buprenorphine, and naltrexone help reduce cravings and withdrawal symptoms associated with opioid addiction.
- Alcohol: Disulfiram, acamprosate, and naltrexone are commonly used to treat alcohol dependency by altering the way alcohol is metabolized and mitigating withdrawal symptoms.
- Nicotine: Patches, gum, lozenges, and other nicotine replacement therapies provide a controlled dose of nicotine to ease withdrawal from smoking without the harmful effects of tobacco.
Research supports the efficacy of MAT in improving patient survival, increasing retention in treatment, and decreasing illicit drug use and other criminal activity among people with substance use disorders. According to the Substance Abuse and Mental Health Services Administration (SAMHSA) 2021 study on Medication and Counseling Treatment, MAT has proven to reduce the need for inpatient detoxification services for these individuals. Studies, such as those conducted by the National Institute on Drug Abuse (NIDA) in 2021 on Medication Assisted Treatment, have shown that when delivered properly, MAT can help patients recover from addiction and can contribute to lowering a person’s risk of contracting HIV or hepatitis C by reducing the potential for relapse.
While MAT is highly effective, it is sometimes met with skepticism due to misconceptions that it replaces one drug with another. Medical and addiction professionals emphasize that the medications used are therapeutic tools, not substitutes for drugs of abuse. They are considered part of a comprehensive therapeutic process when combined with counseling and psychosocial support.
Medication Assisted Treatment is widely implemented in various treatment settings, including outpatient clinics, residential treatment centers, and during aftercare programs, forming a crucial component of modern addiction treatment paradigms. Its use is particularly emphasized in settings where withdrawal management and relapse prevention are critical.
Cognitive Behavioral Therapy (CBT):

Cognitive Behavioral Therapy (CBT) is a widely used evidence-based psychological treatment that has been proven effective for a range of issues including substance use disorders. CBT focuses on identifying and modifying dysfunctional behaviors, emotions, and thoughts through a goal-oriented, systematic approach.
CBT works by helping individuals identify and challenge negative thought patterns and behaviors that contribute to their substance abuse issues and replacing them with healthier, more constructive ones. This therapy empowers individuals to become more aware of their triggers and develop coping strategies to manage and prevent relapses. Techniques often include problem-solving skills, stress management techniques, assertiveness training, and the exploration of the positive and negative consequences of continued drug use.
The effectiveness of CBT in treating substance use disorders is well-documented. A meta-analysis published in the American Journal of Psychiatry (Magill, M. and Ray, L.A., 2009) emphasizes that CBT significantly improves the chances of maintaining sobriety. The National Institute on Drug Abuse (NIDA) highlights in their 2018 study, “Principles of Drug Addiction Treatment: A Research-Based Guide (Third Edition),” that CBT not only helps manage substance abuse but also addresses co-occurring mental disorders by modifying attitudes and behaviors related to drug abuse, thus enhancing the effectiveness of other treatments like medication.
CBT can be conducted in individual sessions with a therapist or in group settings, making it adaptable to a variety of treatment environments. It is typically structured over a series of sessions that build on each other and can be tailored to the needs of the individual, making it a flexible method of treatment that can be adjusted based on the patient’s progress.
One of the primary benefits of CBT is its ability to provide patients with the skills to self-regulate and deal with challenges in recovery long after the completion of treatment. However, its success heavily relies on the active participation of the patient and may require a higher level of commitment and cognitive capability, which can be a limitation for individuals with severe mental impairment or those who have difficulty engaging in psychotherapeutic settings.
Life skills training is closely aligned with Cognitive Behavioral Therapy for addiction as it equips individuals with the tools they need to cope with the stresses and challenges of daily life.
Contingency Management:
Contingency Management (CM) is an evidence-based behavioral therapy that uses motivational incentives and tangible rewards to reinforce positive behaviors such as abstinence from drugs. This method is grounded in the principles of behavioral psychology, particularly operant conditioning, which posits that behavior is more likely to be repeated when it is followed by positive consequences.
In Contingency Management, the rewards are typically contingent upon the submission of drug-free urine samples or other measurable outcomes that demonstrate adherence to treatment goals. The rewards might include vouchers, small cash prizes, or privileges that increase in value with successive achievements, designed to reinforce the desired behaviors progressively.
Research has consistently shown that Contingency Management is highly effective in increasing retention in treatment programs and promoting abstinence from various substances, including opioids, stimulants, and alcohol. A meta-analysis published in the Journal of Consulting and Clinical Psychology (Petry, N.M., 2012) highlights that patients in addiction treatment who participate in CM programs are significantly more likely to achieve sustained abstinence compared to those receiving standard care without incentives. The National Institute on Drug Abuse (NIDA) 2018 study “Principles of Drug Addiction Treatment: A Research-Based Guide (Third Edition).” confirms the efficacy of CM in improving treatment outcomes for substance use disorders.
Despite its proven effectiveness, CM has sparked some debate due to concerns about the ethical implications of using monetary or material rewards in medical treatments and the sustainability of behavior change once the incentives are removed. Critics argue that while CM can effectively initiate behavior change, it might not foster intrinsic motivation for long-term recovery. However, proponents suggest that the immediate benefits of decreased drug use and increased treatment engagement justify the approach, especially as a bridge to more sustainable recovery efforts.
Contingency Management is increasingly incorporated into various treatment settings, including outpatient clinics, residential programs, and VA hospitals, often in combination with other therapeutic interventions like cognitive-behavioral therapy (CBT) and medication-assisted treatment (MAT). Its application has been particularly noted in treatments where adherence is challenging but critical for success, such as methadone maintenance programs for opioid addiction.
Motivational Interviewing (MI) for Addiction Treatment
Motivational Interviewing (MI) is a client-centered, directive therapeutic approach aimed at enhancing intrinsic motivation to change by exploring and resolving ambivalence. It is particularly effective in treating substance use disorders, where motivation can be a significant barrier to entering recovery.
MI operates under the premise that the responsibility and capability for change are within the client. This method involves an empathetic and accepting counselor who encourages individuals to talk about their need for change and their own reasons for it. The technique focuses on engaging clients through open-ended questions, reflective listening, and affirmations that promote a discussion about change based on the client’s own values and concerns.
Research has consistently supported the efficacy of Motivational Interviewing in addiction treatment. A study highlighted in the Journal of Substance Abuse Treatment (Hettema, J., Steele, J., & Miller, W.R., 2005) found that MI significantly improves treatment engagement and adherence, thereby increasing the likelihood of successful outcomes. The National Institute on Drug Abuse (NIDA) in its 2012 guide, “Principles of Drug Addiction Treatment,” emphasizes that MI is effective not only in initiating treatment but also in reducing the severity of relapses in those who do return to substance use.
Motivational Interviewing can be used as a standalone treatment or as a precursor to other therapeutic interventions. It is typically brief, consisting of one to four sessions, and can be integrated into a variety of treatment settings, including outpatient clinics, residential treatment centers, and hospital systems. MI is also used to enhance engagement in more structured therapies such as CBT and MAT.
The strength of Motivational Interviewing, MI lies in its flexibility and client-centered nature, which can significantly enhance patient engagement and empowerment. However, its effectiveness can be limited by the practitioner’s skill in maintaining a non-confrontational and supportive environment. It requires skilled therapists who are adept at guiding rather than directing conversations, a challenge that may not suit all therapeutic contexts.
What Are The Types of Treatment Services and Therapies Offered In Addiction Treatment Programs?

Addiction treatment programs are complemented by therapies and services aimed at holistic recovery.
- Individual and Group Counseling to tackle personal issues and shared experiences.
- Educational and Vocational Services to support continued education and enhance job skills.
- Life Skills Training to help clients manage daily stress and improve self-esteem.
- Mental Health Treatment for those with co-occurring mental disorders, treated alongside substance use.
- Family Services to educate and involve family members in the recovery process.
- Continuing Care plans to support the transition back to everyday life after formal treatment.
The ultimate goal of these treatments and services is not just to cease substance use but to improve the overall quality of life, supporting success in personal and professional spheres, and fostering healthy relationships and a supportive social environment.
What Are Specialized Addiction Treatment Types?

Specialized treatments target individuals with unique needs that cannot be fully addressed by more traditional therapy options. The specialized addiction treatment types are listed below:
Dual Diagnosis: As mentioned earlier, dual diagnosis is crucial for those who experience substance abuse along with another mental health disorder. In cases involving trauma and PTSD, dual diagnosis can provide a more comprehensive treatment plan that addresses both issues concurrently.
Mental Health Treatment: Treating the mental health condition alongside addiction is critical for dual diagnosis. Failure to address the mental illness can lead to relapse, and untreated addiction can exacerbate mental health symptoms.
Family Integration: When dealing with specialized treatments like dual diagnosis, family involvement becomes crucial. The family program’s goal is to provide opportunities to increase understanding of co-occurring disorders and help in stress management and communication. Addiction often affects more than just the individual; it can disrupt family dynamics and relationships as well. Family therapy programs involve loved ones in the treatment process, teaching communication skills, and fostering understanding and reconciliation.
Trauma-Informed Care: Trauma-informed care is an approach that acknowledges the prevalence and impact of trauma in the lives of those seeking addiction treatment. PTSD can lead to self-medication, creating a vicious cycle where substance abuse exacerbates PTSD symptoms. Specialized treatments often employ a multi-disciplinary approach that includes both medication and therapy to address both issues. Trauma treatment within the context of drug addiction aims to avoid re-traumatization and create a setting where the individual feels safe to engage in the recovery process.
Demographic-Based Treatments: These could include treatments for individuals who are deaf and hard of hearing, LGBTQ+-focused therapies, gender-specific treatment approaches, and treatments focused on cultural sensitivities or by profession. For instance, there are different professional treatment approaches for doctors, lawyers, and discreet options for celebrities.
What Are The Alternative Addiction Treatment Options?

The alternative addiction treatment therapies are listed below:
- Holistic Treatments: Beyond traditional medical and psychological interventions, holistic treatments aim to address the person as a whole—mind, body, and spirit. Yoga, meditation, and acupuncture are some of the techniques often employed in this modality. The goal of holistic therapy is to restore balance, thereby giving the individual tools to maintain sobriety by reducing stress and increasing well-being.
- Educational and Vocational Services: Holistic treatments aren’t limited to physical and emotional well-being. Educational and vocational services can offer complementary benefits, helping individuals to re-integrate into society successfully. (NIH)
- Wellness Groups and Sessions: These interventions range from full workout programs to relaxation techniques, aiming to treat the client holistically.
- Experiential Treatments: Experiential therapy takes individuals out of the talking and thinking modality into the realm of action. This could include adventure therapy, which uses outdoor activities like hiking or rock climbing to foster teamwork, build confidence, and develop problem-solving skills. Equine-assisted therapy is another experiential method for treating addiction where interaction with horses is used to mirror and explore emotional states and behavioral patterns.
- 12-Step and Self-Help Programs – Peer Recovery: Derived from the Alcoholics Anonymous (AA) model, 12-step programs are community-based, peer-led support groups. These programs provide a structured environment in which participants progress through 12 steps that focus on admitting powerlessness over the addiction and seeking guidance from a higher power. In addition to AA, there are other variations like Narcotics Anonymous (NA) and SMART Recovery, which is a self-management program.
What Are The Different Levels Of Intensity For Addiction Treatment?
The intensity and duration of addiction treatment can vary significantly, depending on a multitude of factors such as the severity of the addiction, co-occurring mental health disorders, and the specific substances involved. These two elements—intensity and duration—are key considerations in tailoring a treatment plan that best suits an individual’s unique needs.
Intensity refers to the level of medical and therapeutic intervention required and can range from outpatient services to medically managed intensive inpatient services. Intensity levels are also marked by:
- Frequency of sessions: How often a patient undergoes therapy, counseling, or medical check-ups and the setting treatment is administered in (residential vs outpatient).
- Depth of therapy: The complexity and scope of therapies, including the range of issues being addressed in treatment.
- Medical supervision: The extent of medical oversight and intervention, particularly for detox and medication management.
The “Continuum of Care” is an integrated framework of treatment modalities designed to cater to the varied needs of individuals suffering from addiction with different levels of intensity based on the symptoms that are present. This dynamic approach to treatment allows patients to enter and transition between levels of care based on their evolving needs. As delineated by Mee-Lee and Shulman (2003), an effective continuum of care is characterized by seamless transfers between treatment levels, consistent treatment philosophies across those levels, and efficient handling of client records. Furthermore, the American Society of Addiction Medicine (ASAM) has structured this continuum into five primary levels.
Level 0.5: Early Intervention Services: At this initial stage, the focus is on identifying and addressing problematic substance use before it escalates into addiction. This level is a preventive measure designed to nip potential issues in the bud.
Level I: Outpatient Services: Outpatient treatment provides a less restrictive setting and is suited for individuals who can maintain their daily responsibilities while receiving care. It involves periodic therapy sessions and also includes medication management.
Level II: Intensive Outpatient/Partial Hospitalization Services: Comprising sublevels II.1 and II.5, this level offers a more intensive form of outpatient care. Partial hospitalization is included for individuals who require rigorous, structured therapy but not 24-hour inpatient services. Since partial hospitalization takes place throughout the entire day, it is sometimes referred to as “day treatment”.
Level III: Residential/Inpatient Services: Segmented into sublevels III.1, III.3, III.5, and III.7, this level involves residential or inpatient treatment for individuals with severe addiction problems. The setting is controlled, and multi-disciplinary treatment plans are employed to address various facets of addiction. This level of care is commonly referred to as inpatient rehab or inpatient rehabilitation.
Level IV: Medically Managed Intensive Inpatient Services: This is the most intensive form of addiction treatment, designed for patients with acute medical conditions arising from drug addiction. It involves 24-hour medical supervision and intensive therapy. This level of care is commonly referred to as medical detox.
By understanding the continuum of care in addiction treatment, it becomes evident that ‘treatment’ is not a one-size-fits-all approach but a nuanced, multifaceted framework tailored to each individual’s unique needs.
How Can Treatment Change Based on the Stage of the Addiction Cycle and the Severity of the Addiction?
The stage of the addiction cycle and the severity of the addiction are critical factors that healthcare providers consider when determining the most appropriate treatment plan. In the early stages of addiction, when an individual is experimenting with a substance but is not yet dependent, outpatient treatment and counseling can be sufficient to bring about a full recovery. This approach allows the individual to continue with their daily activities while receiving support and education to prevent further progression into addiction.
As the addiction becomes more severe and the individual moves into regular use and dependence, more intensive treatment options are necessary. This could include inpatient treatment, which provides a structured environment for detoxification, medical supervision, and intensive therapy. In the most severe cases, where there are significant physical and mental health risks, long-term residential treatment is recommended. These programs offer extended care, often lasting several months, and focus on treating the addiction as well as any co-occurring disorders.
The treatment plan evolves as the individual progresses through recovery. For example, someone transitioning from an inpatient setting to an outpatient program and then to aftercare services like support groups or sober living homes. The goal is to provide a continuum of care that supports the individual at each stage of the addiction, adapting the treatment approach as their needs change.
What are the different types of addiction treatment?
Addiction treatment encompasses a range of programs and services tailored to meet diverse needs, operating in various settings and with varying intensities. Treatment isn’t just about detoxing, which only addresses the physical symptoms of withdrawal, but also involves a comprehensive approach to tackle the underlying psychological, emotional, and social issues associated with substance use. According to SAMSHA’s guidance on treatment types updated in 2023, some treatments are for specific conditions, while others work for many different conditions. The goal of most treatments is to change thoughts and behaviors, and, if needed, manage physical dependence on drugs or alcohol. You may need more than one type of treatment.
Types of Treatment Programs according to the partnership to end addiction are listed below.
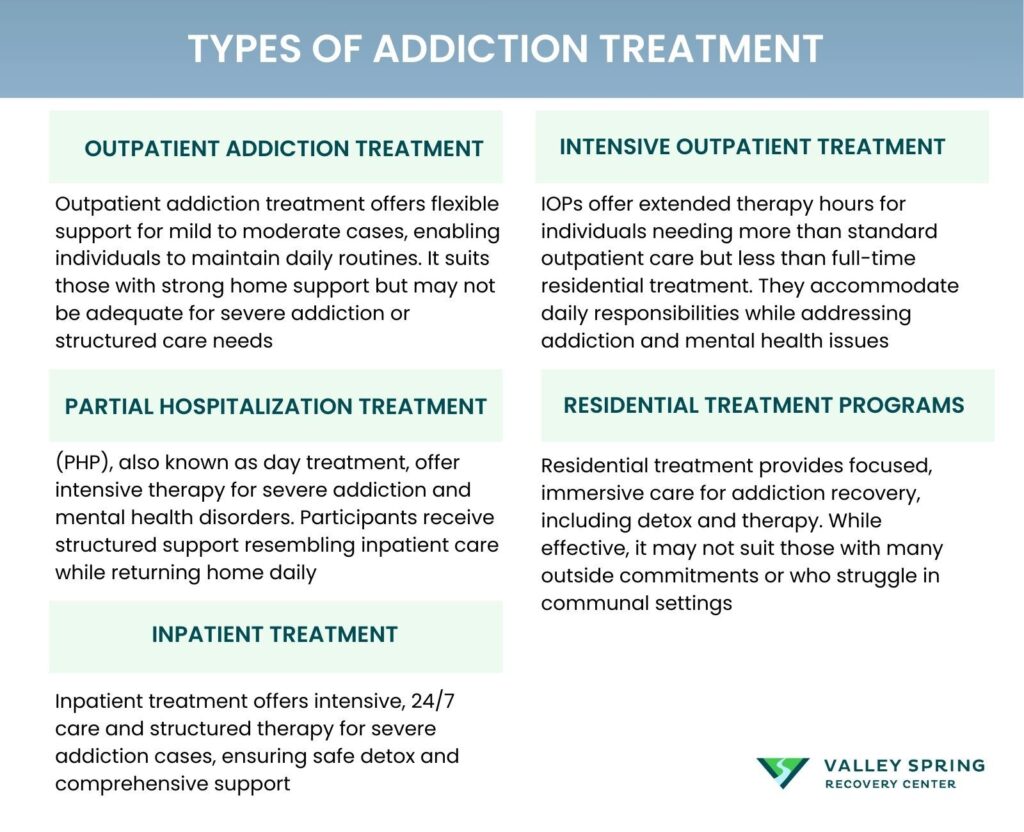
What Is Outpatient Addiction Treatment?
Outpatient addiction treatment provides therapeutic services and support for individuals battling substance use disorders while they continue to live at home. This flexible treatment model allows clients to maintain their daily responsibilities such as work, school, or family commitments.
Outpatient programs typically require attendance at a treatment facility for up to nine hours per week. During these sessions, clients engage in various forms of therapy, including individual counseling, group therapy, and sometimes educational workshops that address substance abuse. The goal is to integrate treatment into the individual’s daily life, allowing them to apply recovery strategies in real-world settings.
This treatment model is particularly beneficial for those who have mild to moderate addiction issues and a strong support network at home. It allows for a greater balance between treatment and everyday life, providing the necessary support without complete removal from one’s usual environment. Outpatient treatment options can be a cost-effective alternative to inpatient programs, offering essential recovery resources without the need for a residential stay. However, it may not be suitable for individuals with severe addiction or those who require a structured environment to avoid relapse.
What Is Intensive Outpatient Treatment?
Intensive Outpatient Programs (IOP) provide increased treatment, requiring clients to attend 10-20 hours of therapy weekly. These programs are suitable for individuals needing more extensive services than standard outpatient care, offering a higher level of support while still allowing participants to live at home and, in many cases, continue working or attending school.
IOPs serve as a critical step for individuals who need more than just a few hours of therapy a week but who do not require or cannot commit to full-time residential care. These programs typically include multiple therapy sessions each week, along with access to psychiatric care, medical treatment, and holistic therapies.
The structure of IOPs is particularly advantageous for individuals with co-occurring disorders or those who have not succeeded with lower levels of care. The increased treatment hours allow for a more comprehensive approach to address complex issues related to addiction and mental health. IOPs facilitate continued personal responsibilities alongside rigorous treatment, making it a viable option for many seeking recovery. However, IOPs might not provide enough support for those with high-risk addiction profiles or those who struggle with severe impulse control, where a more controlled environment may be necessary.
What Is Partial Hospitalization Treatment?
Partial Hospitalization Programs (PHP), also known as day treatment, offer a rigorous, structured treatment experience where clients attend therapy for four to eight hours per day.
PHP is designed to provide intensive treatment that mirrors the support found in inpatient programs, but participants return home at the end of the day. This setup is ideal for those transitioning from inpatient care or those who require more support than what is offered in outpatient settings.
PHPs are beneficial for treating severe cases of addiction and mental health disorders, providing a level of care that supports significant behavioral changes and medical management. These programs allow for intensive therapy and support while still maintaining a connection to the home environment, which can be crucial for long-term recovery.
PHP is not suitable for individuals who lack a stable living situation or are easily influenced by external triggers due to the less restrictive nature of outpatient programs in comparison to full residential care.
What Are Residential Treatment Programs?
Residential treatment programs involve living at a treatment facility for an extended period, offering a structured and phased approach to addiction recovery.
These programs provide a continuum of care, from detox to various therapeutic interventions, in a residential setting. Treatment typically includes a combination of group and individual counseling, educational sessions, and possibly vocational training, depending on the length of stay.
The immersive nature of residential treatment allows for a focus solely on recovery without the distractions or triggers of everyday life. This environment fosters intensive personal reflection and change, supported by professional staff and a community of peers who share similar challenges. However, the intensive nature and isolation from usual life may not be suitable for those who have significant obligations outside of treatment or who may not adapt well to communal living environments.
What Is Inpatient Treatment?
Inpatient treatment requires individuals to stay at a hospital or clinic, offering around-the-clock care and comprehensive treatment services for addiction.
Inpatient programs are highly structured, providing medical detoxification followed by a series of intensive therapy sessions and other treatment modalities. These programs are typically recommended for individuals with severe addictions or those who require medically supervised detoxification.
The controlled environment of inpatient residential rehab minimizes the risk of relapse during the initial recovery stages and allows for intensive medical and psychological care. Inpatient treatment is often necessary for those who need a stable environment to manage acute symptoms of addiction and withdrawal safely. However, the restrictive environment and potential distance from family and social support networks might not be ideal for everyone, particularly those who may benefit from the less intensive
What Are The Different Symptoms That Require Addiction Treatment?
The different symptoms that require addiction treatment are physical, emotional and psychological symptoms, and behavioral symptoms.
- Physical symptoms are types of symptoms that can signal the requirement for addiction treatment and often serve as the most noticeable indicators of a drug addiction problem. Individuals experience withdrawal symptoms such as physical discomfort or nausea when not using the drug. Additionally, a build-up of tolerance, where increasingly larger doses of the drug are needed to achieve the desired effect, is a significant red flag. Neglected personal hygiene and appearance, as well as recurring health issues like respiratory problems, liver damage, or heart conditions, can also point to the need for immediate treatment.
- Emotional and psychological symptoms can be just as telling as physical ones. Extreme mood fluctuations, including irritability, aggression, or depression, are common. Increased levels of anxiety or paranoid behavior can also be indicative of a deeper issue. Emotional numbness, or a lack of emotional responsiveness, is another sign, along with cognitive impairments such as difficulty in concentration, memory loss, or poor decision-making skills.
- Behavioral symptoms often manifest in various aspects of life and can be quite disruptive. Neglecting responsibilities at work, school, or home is a common sign. Social isolation, where the individual withdraws from social activities and distances themselves from friends and family, is another. Risk-taking behavior, especially when under the influence of drugs, can also indicate a severe problem. Legal issues, such as arrests for possession or driving under the influence, further underscore the need for treatment.
- Interpersonal relationships can also suffer due to drug addiction. Increasing conflicts or arguments with loved ones often occur, along with secrecy and deception as the individual goes to great lengths to hide their drug use. Unexplained financial difficulties, often due to spending on drugs, can be another sign. The loss of a support network, where friends and family distance themselves due to disapproval of the drug use, can be particularly damaging.
| Symptom Type | Symptoms |
|---|---|
| Physical | – Withdrawal symptoms (e.g., physical discomfort, nausea) – Increased tolerance (needing larger doses) – Neglected personal hygiene and appearance – Recurring health issues (e.g., respiratory problems, liver damage, heart conditions) |
| Emotional and Psychological | – Extreme mood fluctuations (irritability, aggression, depression) – Increased anxiety or paranoia – Emotional numbness – Cognitive impairments (difficulty concentrating, memory loss, poor decision-making) |
| Behavioral | – Neglecting responsibilities (work, school, home) – Social isolation – Risk-taking behavior – Legal issues (arrests for possession, DUI) – Increasing conflicts with loved ones – Secrecy and deception – Unexplained financial difficulties – Loss of support network |
What Happens When Treatment Is Not Successful?
Failure in addiction treatment, often manifested as an inability to remain abstinent, resulting in relapse, is not an uncommon scenario. It’s critical to understand that addiction treatment is a complex and ongoing process that doesn’t guarantee immediate or permanent success. Despite the setbacks, a relapse should not be viewed as an outright failure but rather as a pivotal moment that requires a reassessment and recalibration of the treatment plan.
Frequently Asked Questions (FAQs) About Addiction Treatment
What Role Does the Family Play in Addiction Treatment?
Family involvement is crucial, especially in specialized treatments like Dual Diagnosis or trauma-informed care. Families are often integrated into the treatment program through educational sessions and counseling. Involvement helps family members understand addiction as a chronic illness and improve overall communication and functioning within the family unit.
What is Trauma-Informed Care?
Trauma-Informed Care is a treatment approach that recognizes the widespread impact of trauma on those seeking addiction treatment. The aim is to create a safe and supportive environment that avoids re-traumatizing the individual. This approach is especially beneficial for individuals who have experienced significant trauma and have PTSD symptoms alongside substance abuse issues.
How Does Group Counseling Differ From Individual Counseling?
In individual counseling, the patient meets one-on-one with a therapist to explore personal issues that might be difficult to discuss in a group setting. On the other hand, group counseling comprises six to ten participants and is facilitated by one or two counselors. The group format allows individuals to share their experiences, struggles, and coping strategies, fostering a sense of community and shared understanding.
What is Dual Diagnosis and Why is it Important?
Dual Diagnosis is a specialized treatment approach for individuals who suffer from both a mental health disorder, such as anxiety or depression, and substance abuse. Treating only one condition can often lead to a relapse or exacerbation of the untreated issue. In Dual Diagnosis, the focus is on treating both disorders simultaneously, increasing the chances of a successful, long-term recovery.
What is the main goal when evaluating the effectiveness of treatment approaches for substance use disorders?
The primary focus in evaluating the effectiveness of various treatment approaches for substance use disorders is generally abstinence or at least a clinically meaningful reduction in substance use. Other important outcomes usually assessed include treatment retention and associated problems like psychiatric severity, medical issues, legal concerns, family/social relations, and job/vocational functioning. Although there is some variability in how these criteria are measured, most researchers agree on these indicators and standard assessment procedures. (Psychiatr Clin North Am, vol. 26)
What Are the Costs Associated with Addiction Treatment?
The costs of addiction treatment can vary widely depending on the type of treatment, location, and duration. While insurance covers some costs based on plan type, additional out-of-pocket expenses are likely. It’s essential to inquire about costs upfront and explore payment options.
What Are the Success Rates of Different Addiction Treatments?
Success rates can vary depending on the type of addiction, the individual’s commitment to recovery, and the quality of the treatment program. Evidence-based treatments like CBT and MAT generally have higher success rates, but individual outcomes can differ.
How Do Inpatient and Outpatient Treatments Differ?
Inpatient treatment involves staying at a specialized facility for a specific period, usually ranging from 30 to 90 days, for intensive therapy and medical supervision. Outpatient treatment allows individuals to live at home while attending scheduled therapy sessions, offering more flexibility but generally less supervision.
Are Medications Used in Addiction Treatment?
Yes, medication-assisted treatment (MAT) is often used in conjunction with behavioral therapies. Medications like Methadone, Buprenorphine, and Naltrexone are commonly used to manage withdrawal symptoms and cravings, particularly for opioid addiction.
What is the Importance of Aftercare in Addiction Treatment?
Aftercare is a crucial component of long-term recovery and often involves ongoing therapy, support groups, and sometimes sober living environments. It aims to provide continued support and resources to prevent relapse.
How Effective is Holistic Treatment?
Holistic treatment approaches, which may include practices like yoga, meditation, and nutritional counseling, are increasingly recognized for their potential to support traditional therapies. However, their effectiveness can vary from person to person and should not replace evidence-based treatments.
Where to get addiction Treatment
Addiction treatment can occur in a drug rehab center or outpatient program. Intensity levels can vary, with outpatient addiction treatment and inpatient services offering different degrees of support needed to address the step in the addiction cycle, both of which come with their own set of protocols and payment options. There are also community-based programs like Alcoholics Anonymous (AA) or SMART Recovery exist as supportive networks, providing ongoing maintenance and relapse prevention strategies.
Whether it’s evidence-based methods like Cognitive Behavioral Therapy and Medication-Assisted Treatment or more holistic and experiential therapies like yoga and equine-assisted therapy, each approach serves to meet unique needs. These methods often intersect with medical and psychiatric services, where professionals such as psychiatrists, medical providers, and registered nurses work in concert to address the multifaceted nature of addiction.
Outpatient Addiction treatment is available in Northern New Jersey for individuals struggling with addiction. Call our 24/7 hotline or verify your insurance online to get help immediately.
Sources
- Suchman, Nancy E., et al. “The Impact of Substance Use Disorders on Families and Children: From Theory to Practice.” Social Work in Public Health, vol. 26, no. 3-4, 2011, pp. 194–205, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2935644/. Accessed [September 6th, 2023].
- Types of Addiction Treatment.” Partnership to End Addiction, https://drugfree.org/article/types-of-addiction-treatment/. Accessed [September 7th, 2023].
- McGovern, Mark P., and Kathleen M. Carroll. “Evidence-based practices for substance use disorders.” Psychiatr Clin North Am, vol. 26, no. 4, Dec. 2003, pp. 991-1010. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3678283/. Accessed [September 8th, 2023].
- Center for Substance Abuse Treatment. Substance Abuse: Clinical Issues in Intensive Outpatient Treatment. Rockville (MD): Substance Abuse and Mental Health Services Administration (US); 2006. (Treatment Improvement Protocol (TIP) Series, No. 47.) Chapter 3. Intensive Outpatient Treatment and the Continuum of Care. Available from: https://www.ncbi.nlm.nih.gov/books/NBK64088/
- Magill, M. and Ray, L.A. “Cognitive Behavioral Therapy and the Treatment of Addiction.” American Journal of Psychiatry, 2009.
- National Institute on Drug Abuse (NIDA). “Principles of Drug Addiction Treatment: A Research-Based Guide (Third Edition).” NIDA, 2018.
- Substance Abuse and Mental Health Services Administration (SAMHSA). “Medication and Counseling Treatment.” SAMHSA, 2021.
- National Institute on Drug Abuse (NIDA). “Medication-Assisted Treatment (MAT).” NIDA, 2021.
- Petry, N.M., “Contingency Management for Substance Abuse Treatment: A Guide to Implementing This Evidence-Based Practice,” Routledge, 2012.
Dr. Michael Olla
All author postsShare This Post