Xylazine is supposed to be used by veterinarians as anesthesia for animals, not humans, yet it’s still showing up in drug tests and autopsies across the United States. A recent study conducted Russell E, Sisco E, Thomson et al., surveyed eight syringe service programs in Maryland discovered xylazine in nearly 80% of opioid-containing drug samples.
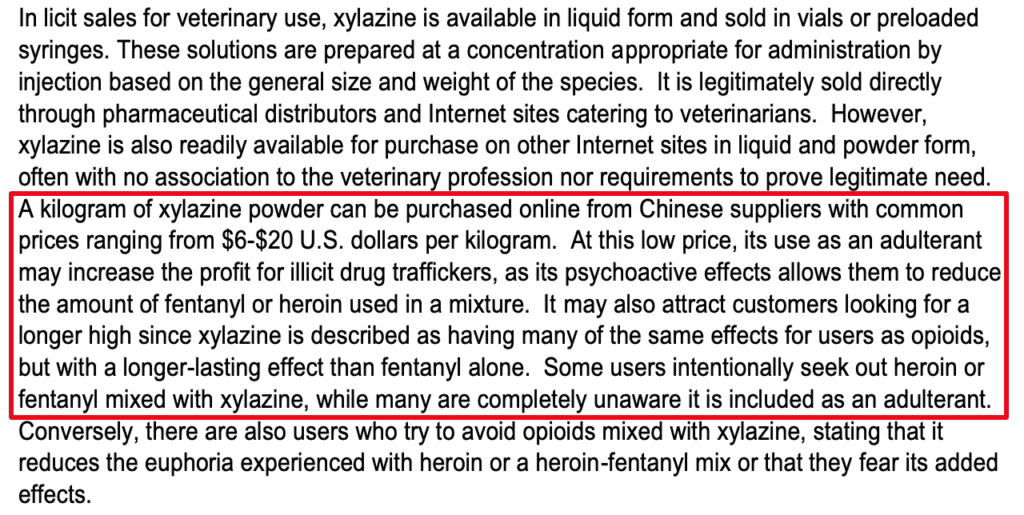
Xylazine is very easy to obtain and can be ordered online from China for $6 a Kilo, as reported by the DEA in their publication ‘The Growing Threat of Xylazine and its Mixture with Illicit Drugs.’ According to the CDC, the Xylazine overdose rate is rapidly increasing in the United States with 107,081 recorded drug overdose deaths involving xylazine and opioids like heroin and fentanyl in 2022 alone. A growing portion of these tragedies occur when xylazine is mixed with other drugs. For instance, in Philadelphia, Pennsylvania, xylazine was present in 31% of heroin and/or fentanyl overdose deaths in 2019, as stated in the Clinical Chemicas 2021 report.
What is Xylazine?
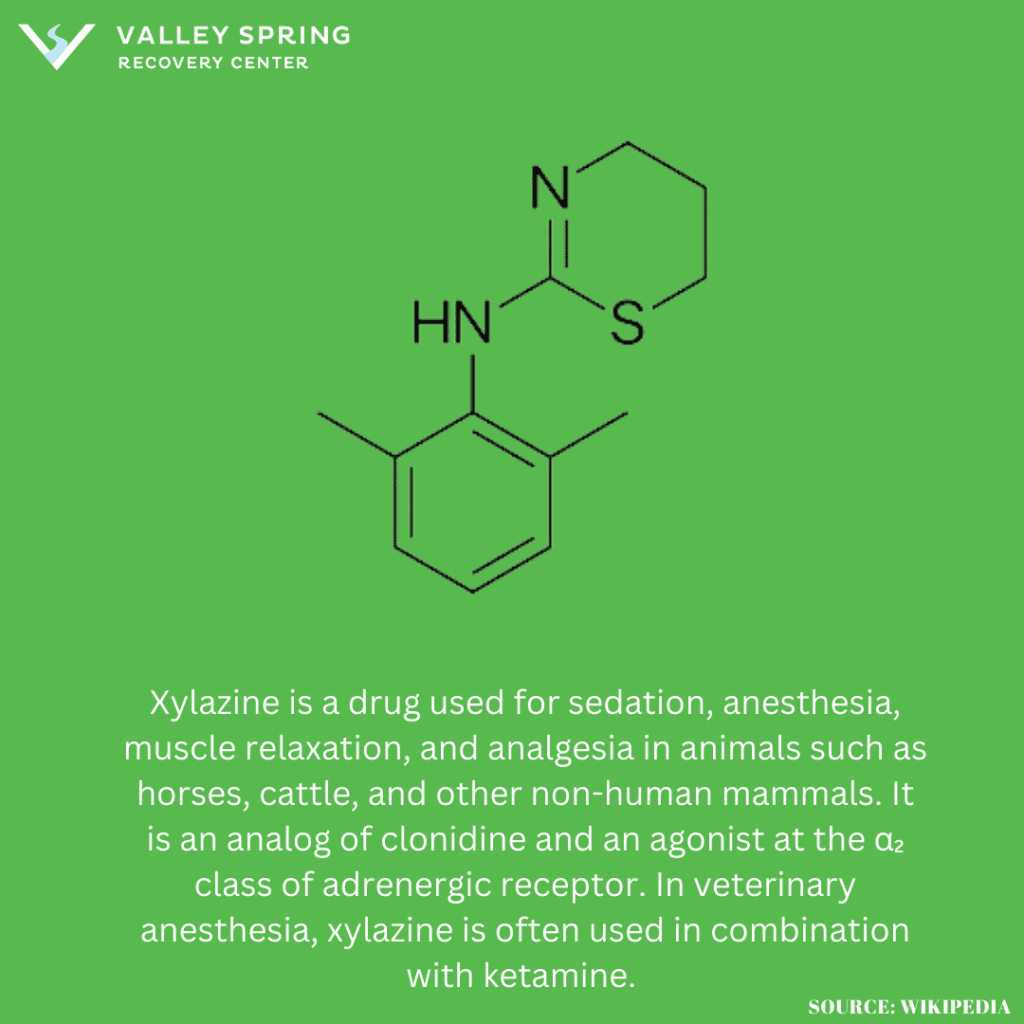
Xylazine is a tranquilizer drug used for sedation, anesthesia, muscle relaxation, and analgesia in animals. Xylazine acts as a central nervous system depressant that causes drowsiness and suppresses breathing, heart rate, and blood pressure to dangerously low levels. It acts as an analog of Clonidine and can be fatal when mixed with opioids like Fentanyl. It was originally developed for use on animals and is not approved for human use. The CDC lists Xylazine as a Schedule I drug.
Clinical Chemicas 2021 report found that xylazine was present in 31% of heroin and/or fentanyl overdose deaths in Philadelphia PA in 2019 which shows a fast increase in overdose deaths when Xylazine is mixed with Opiates or other depressants.
The slang terms for Xylazine are tranq or tranq dope.
What Are The Effects Of Xylazine Use In Humans?
The effects of xylazine in humans are listed below according to NIDA:
- Sedation and Drowsiness: Similar to its effects on animals, xylazine can cause profound levels of sedation and drowsiness.
- Respiratory Depression: It exacerbates the risk of respiratory arrest, particularly when combined with opioids.
- Hypotension and Bradycardia: These cardiovascular effects can be dangerous, leading to fainting or collapse.
- Skin Ulcers and Lesions: With repeated use, particularly via injection, xylazine has been associated with severe skin ulcers and soft tissue infections.
- Overdose Risk: There is a high risk of overdose, especially when users are unaware of its presence in adulterated drugs.
A personal story from the Author on the effects of Xylazine:
I have never taken Xylazine, however, I took Clonidine (which is like Xylazine) after shoulder surgery in college after a surgery and I slept for almost 24 hours afterward and could barely open my eyes because I was so tired. I would imagine taking it with an opiate that also lowers your blood pressure and heart rate is extremely dangerous.
George Kocher
To further highlight the seriousness of the problem, when you google Xylazine, articles about overdoses come up from NIH, the DEA, and the CDC.
Why Are Xylazine And Fentanyl Dangerous When Combined?
Xylazine used in combination with fentanyl, creates a particularly lethal cocktail due to the depressant qualities of Xylazine and Fentanyl individually that are amplified when taken simultaneously. The lethality of this combination stems from their pharmacological actions which depress the central nervous system. Fentanyl is 50 to 100 times more potent than morphine and heroin and primarily contributes to respiratory depression, which can lead to fatal overdoses. When combined with Xylazine, which is not an opioid but still depresses the central nervous system, the risk of fatal respiratory failure increases exponentially.
The White House’s Office of National Drug Control Policy has recognized the adulteration of fentanyl with Xylazine as an emerging and serious threat. This combination represents a grave concern for public health officials and law enforcement, as it complicates treatment for overdose and heightens the risk of death among users, often unbeknownst to them. The alarming spread of Xylazine in the illicit opioid market magnifies the already dire opioid epidemic, demanding urgent attention and response from both healthcare providers and policymakers.
What are the causes of Xylazine Overdose?
The causes of Xylazine-related overdoses and fatalities stem from synergistic effects that drastically lower blood pressure and cause respiratory depression, as well as heart rate deceleration according to NIDA.
The increasing rate of Xylazine overdoses can be attributed to its increasing availability and low costs making it an attractive additive for those looking to increase the effects of opioids, often without fully understanding the risks involved.
The risks of overdose increase drastically when combined with other drugs. For instance, in Philadelphia, Xylazine was detected in a startling 31% of the 858 fatal heroin and/or fentanyl overdose cases in 2019, a significant increase from less than 2% between 2010 and 2015. Furthermore, in Maryland, approximately 80% of drug samples containing opioids tested positive for Xylazine at various syringe service programs between 2021 and 2022. This indicates not only the drug’s widespread presence but also its integration into the illicit drug supply.
What Are the Symptoms of a Xylazine Overdose?
The symptoms of a Xylazine overdose closely mirror its intended effects but to a much more severe degree. These can include extreme drowsiness, respiratory depression, significantly lowered heart rate, hypotension (dangerously low blood pressure), and even coma. In severe cases, an overdose can lead to death, particularly when combined with other substances that depress the central nervous system.
How Do People Take Xylazine If It’s Really Made for Elephants?
Xylazine is used in veterinary medicine for a range of animals, not just elephants. In illicit human use, it is often administered in the same ways as other injectable drugs, such as intravenously or intramuscularly. The drug may also be snorted or ingested, although these methods are less common. Because Xylazine is formulated for animals, the dosages are far higher than what would be considered safe for human use, making any form of consumption extremely risky.
Does Xylazine Rot Your Skin Like Krokodile?
According to the DEA and CDC, Xylazine can cause severe skin ulcers when injected as well as severe wounds, including necrosis which is the rotting of human tissue which can end in amputation. However, the effects of Krokodile are more severe and common when injected. Krokodile is a semi-synthetic opiate that is made from drugs and household items that has effects 8-10 times stronger than morphine. stronger than heroin or fentanyl and also can commonly result in skin deterioration and other extreme effects which made new headlines when it first became popular in Russia. Some of the effects of Krokodile listed by California Poison Control include localized injuries as well as pneumonia, sepsis, meningitis, osteomyelitis and osteonecrosis, neurologic injury (such motor and memory impairment), ulceration and tissue damage at sites distant from the injection site, liver injury, renal impairment, and death. Drugs.com states that it’s common for Krokodile to result in serious vein damage, soft tissue infections, necrosis, and gangrene. The bodily impact of Krokodile is more severe than Xylazine, although injection of either drug can result in severe skin infections and rotting tissue.
Does Xylazine Lower Blood Pressure like Clonodine or Xanax?
Xylazine can cause a significant decrease in blood pressure and a lowering of the heart rate. The drug also causes sedation and anesthesia, respiratory depression, and muscle relaxation which can be dangerous when mixed with other drugs. Xylazine presents dangerous effects to blood pressure similar to how Xanax can lower blood pressure when mixed with other drugs and result in an overdose.
When did Xylazine first show up and become popular?
Xylazine was first synthesized in 1962 by Bayer Pharmaceutics and has been available for veterinary use for several decades, but its appearance in human drug samples is a more recent phenomenon. There were scattered reports of Xylazine use in drug users over the past few decades (Ruiz-Colón et al., 2014; Forrester, 2016) but it became more popular in Puerto Rico in the early 2000s before making its way into the United States(Reyes et al., 2012). Since then, Xylazine use in the United States has increased at an alarming rate, one study from 10 US cities showed xylazine was involved in less than 1% of drug overdose deaths in 2015 and in nearly 7% in 2020 (Friedman J, Montero F, Bourgois P, et al. Drug and alcohol dependence. 2022).
What Is Xylazine Good For?
Xylazine is primarily used as a sedative, analgesic, and muscle relaxant in veterinary medicine. It is commonly employed in the sedation of large animals such as horses, cattle, and deer, as well as smaller animals like dogs and cats. Here’s a breakdown of its main uses:
Xylazine induces a calm and relaxed state in animals, making it easier for veterinarians to perform examinations, treatments, or surgical procedures. It is often used in combination with other anesthetics to provide a more comprehensive anesthetic protocol.
The drug has pain-relieving properties, making it useful for minor surgical procedures where pain management is necessary.
Xylazine helps to relax the skeletal muscles, facilitating procedures that require an absence of muscle tension, such as the setting of fractures or the insertion of catheters.
In some cases, xylazine is used to facilitate diagnostic procedures like radiography by keeping the animal still and relaxed. In higher doses, xylazine can be used for euthanasia, although this is generally not its primary application and is usually combined with other agents for this purpose.
What are the withdrawal symptoms associated with Xylazine misuse?
Xylazine is a drug primarily used as a sedative, analgesic, and muscle relaxant in veterinary medicine. It is not approved for human use but has been misused recreationally. Xylazine itself is not generally considered to be physically addictive in the way that opioids or alcohol are, and thus, does not have severe withdrawal symptoms when used alone. The most common use of xylazine is in combination with other substances, in which case, it can be extremely dangerous.
Misuse of xylazine can lead to a range of adverse health effects, including respiratory depression, bradycardia (slow heart rate), hypotension (low blood pressure), and even death, particularly when combined with other depressants like opioids or alcohol. However, when used alone, xylazine is not recognized as a substance that produces physical dependence.
How to Overcome Xylazine Addiction
Overcoming xylazine addiction necessitates treating the primary substance of abuse, such as fentanyl or heroin, as xylazine dependency is typically secondary to addiction to these other opiates. A comprehensive diagnostic assessment is crucial for identifying the specific addiction and any co-occurring mental or behavioral disorders that also need treatment, with the most effective approach being a holistic regimen that combines medical and therapeutic interventions. After detox, ongoing treatment through a Partial Hospital Program or intensive outpatient program to support ongoing recovery and sobriety.
Sources
https://www.dea.gov/alert/dea-reports-widespread-threat-fentanyl-mixed-xylazine
https://nida.nih.gov/research-topics/xylazine
https://www.dea.gov/sites/default/files/2022-12/The%20Growing%20Threat%20of%20Xylazine%20and%20its%20Mixture%20with%20Illicit%20Drugs.pdf
https://www.sciencedirect.com/science/article/abs/pii/S037687162200117X?via%3Dihub
https://g.co/kgs/jPQ52U
Share This Post