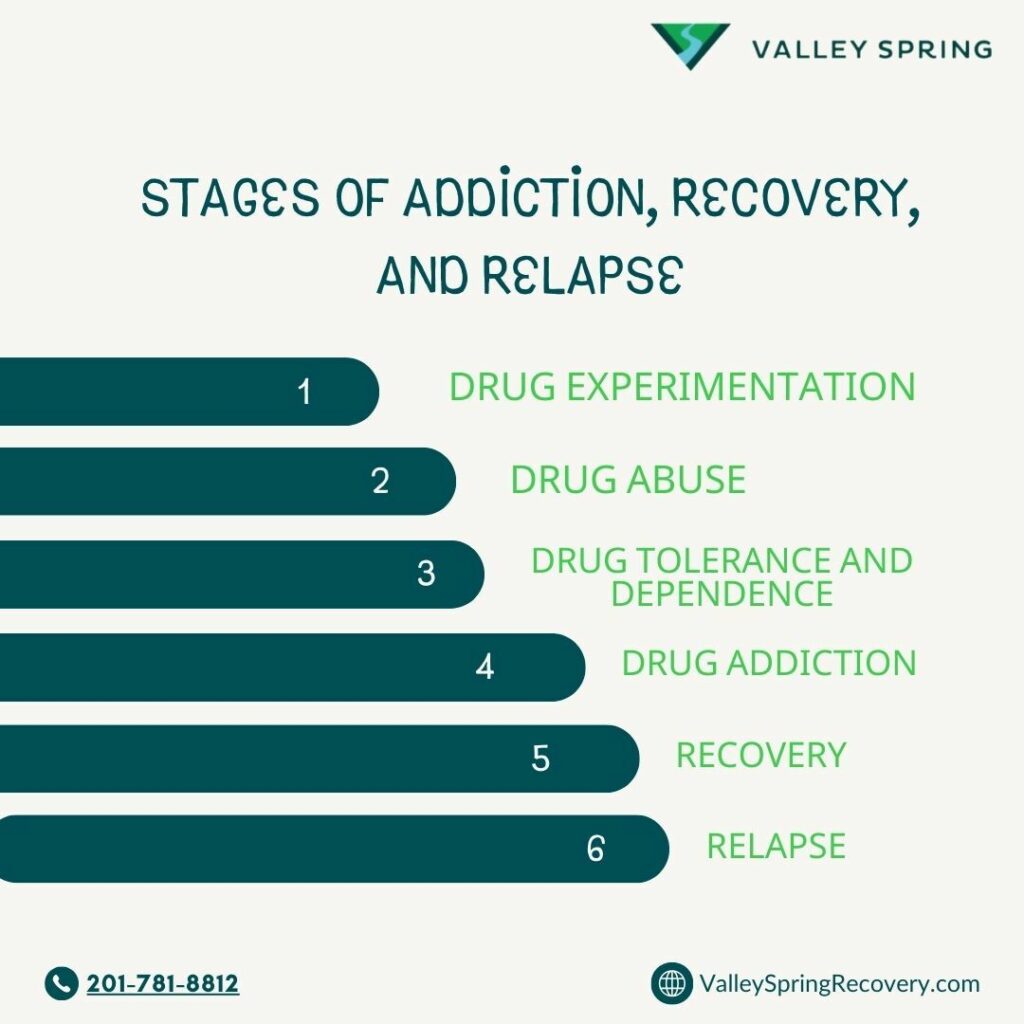
Addiction is a chronic and multifaceted condition marked by the compulsive use of substances or behaviors, despite the detrimental consequences they may bring. This condition progresses predictably through several stages: experimentation, drug abuse, drug tolerance or physical dependence, active addiction, recovery, and sometimes relapse.
Variability in Addiction Manifestation
Addiction’s manifestation is not uniform; it varies significantly among individuals. Research from the National Institute on Drug Abuse (NIDA) suggests that genetic factors contribute to 40%-60% of an individual’s susceptibility to addiction, affecting the severity and progression of the disease (NIDA, 2020). Furthermore, the method of substance use can greatly influence the development and intensity of addiction, necessitating personalized treatment approaches.
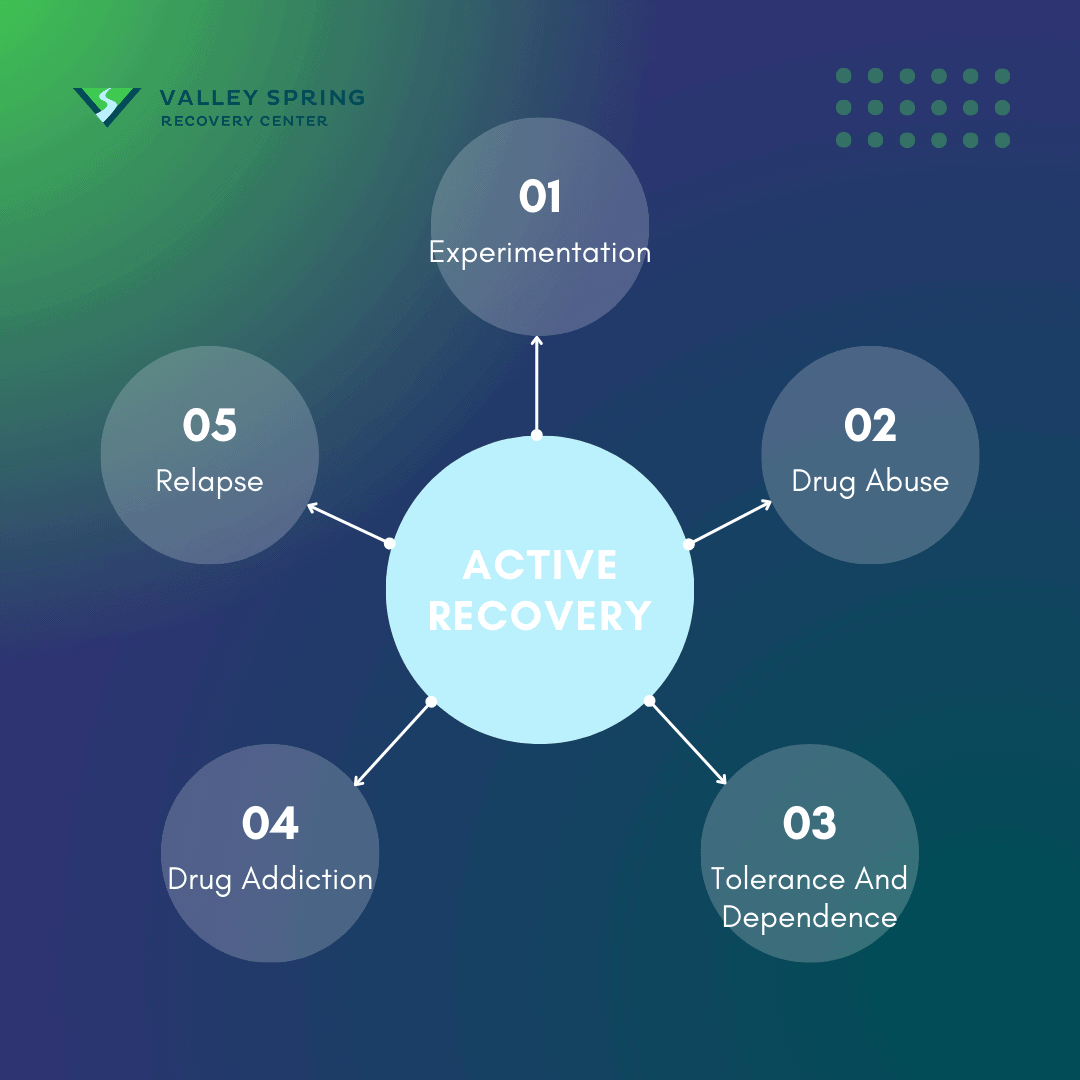
Stages of Addiction
- Experimentation: Begins with occasional use of harmful substances to achieve a high. Not all experimenters progress beyond recreational use.
- Drug Abuse: As use becomes more frequent and excessive, the adverse effects on health and wellbeing intensify.
- Tolerance and Dependence: Users may develop a tolerance, needing increasingly larger doses to achieve the same effects, leading to physical and mental dependence.
- Active Addiction: Characterized by continued substance use despite harmful consequences.
- Recovery: Achievable through comprehensive addiction treatment that addresses all symptoms of the underlying addiction.
- Relapse: Occurs when an individual ceases to maintain their recovery efforts and reverts to previous levels of substance use.

This article has been enhanced with input from the Medical Director and Addiction Psychiatrist at Valley Spring Recovery Center, Dr. Michael Olla.
Check the end of each section for extra information from him.
Importance of Accurate Terminology in Addiction

It’s crucial to differentiate between commonly used terms such as “addiction,” “abuse,” and “dependence,” which are often used interchangeably yet fail to capture the complexity of substance use disorder. The term “substance use disorder” offers a more comprehensive understanding without the negative connotations associated with other terms, although it does not detail the severity or progression of the addiction cycle. Thus, we utilize stages to clarify these terms and provide insight into the progression of substance use disorders as defined by Doctor Michael Olla, addiction Psychiatrist and editor of this article. Recognizing the stages of addiction is vital for understanding its complex nature and the need for tailored treatment strategies. With proper treatment and support, recovery from addiction is possible, offering hope to those affected by this challenging condition.
1. 1st Use (Experimentation)

Drug experimentation is the initial phase in the progression toward active drug addiction. It involves trying a substance, often out of curiosity or peer influence, with the primary goal of experiencing its numbing or euphoric effects. Drug experimentation can be a one-time occurrence or involve sporadic use without necessarily developing an addiction.
This phase involves the occasional use of substances to achieve a euphoric effect. Data from the Substance Abuse and Mental Health Services Administration (SAMHSA) indicates that in 2019, approximately 139.8 million Americans aged 12 or older were current alcohol users, with many beginning through experimental use (SAMHSA, 2020).
Although experimenting with drugs doesn’t mean you’ll become addicted, it often opens the door to other levels in the drug addiction cycle, like drug abuse, tolerance, and dependence, which can then lead to full-blown drug addiction.
Why do people experiment with drugs and use them in the first place?
Experimentation with drugs often marks the initial step in a person’s interaction with substances, which can sometimes lead to abuse and dependency. While many might categorize any drug use as abuse, it is essential to differentiate between experimentation and habitual use because the motivations and contexts can vary significantly.
Key Reasons for Drug Experimentation Include:
- Curiosity: Many people first try drugs out of curiosity to experience their effects firsthand.
- Peer Pressure: Especially among teenagers and young adults, peer influence is a powerful factor in deciding to try drugs.
- Social Integration: Drugs are often used within social settings to enhance camaraderie or integrate into a particular social group.
- Recreational Experience: The pursuit of pleasure and heightened experiences at parties or gatherings can prompt initial drug use.
- Stress Relief: Individuals may turn to drugs as a coping mechanism to relieve stress or escape from daily pressures.
- Risk-Taking Behavior: Some people are naturally inclined towards sensation-seeking and risk-taking behaviors, which include experimenting with drugs.
- Cultural Norms: In certain cultures or communities, drug use may be more normalized and less stigmatized, influencing individuals to partake.
- Media and Pop Culture Influence: Portrayals of drug use in media and pop culture can glamorize the act, making it appear appealing and acceptable.
- Self-Medication: Some individuals use drugs to manage symptoms of mental health issues or physical pain, often without medical guidance.
- Self-Exploration: People might use drugs to explore altered states of consciousness or deepen their understanding of self.
Understanding drug and alcohol experimentation motivations is crucial for addressing the root causes of drug use and effectively supporting individuals at risk of developing substance abuse disorders. Recognizing that experimentation does not always lead to addiction can help in creating targeted interventions that respect individual experiences while promoting healthier choices.
2. Drug Abuse
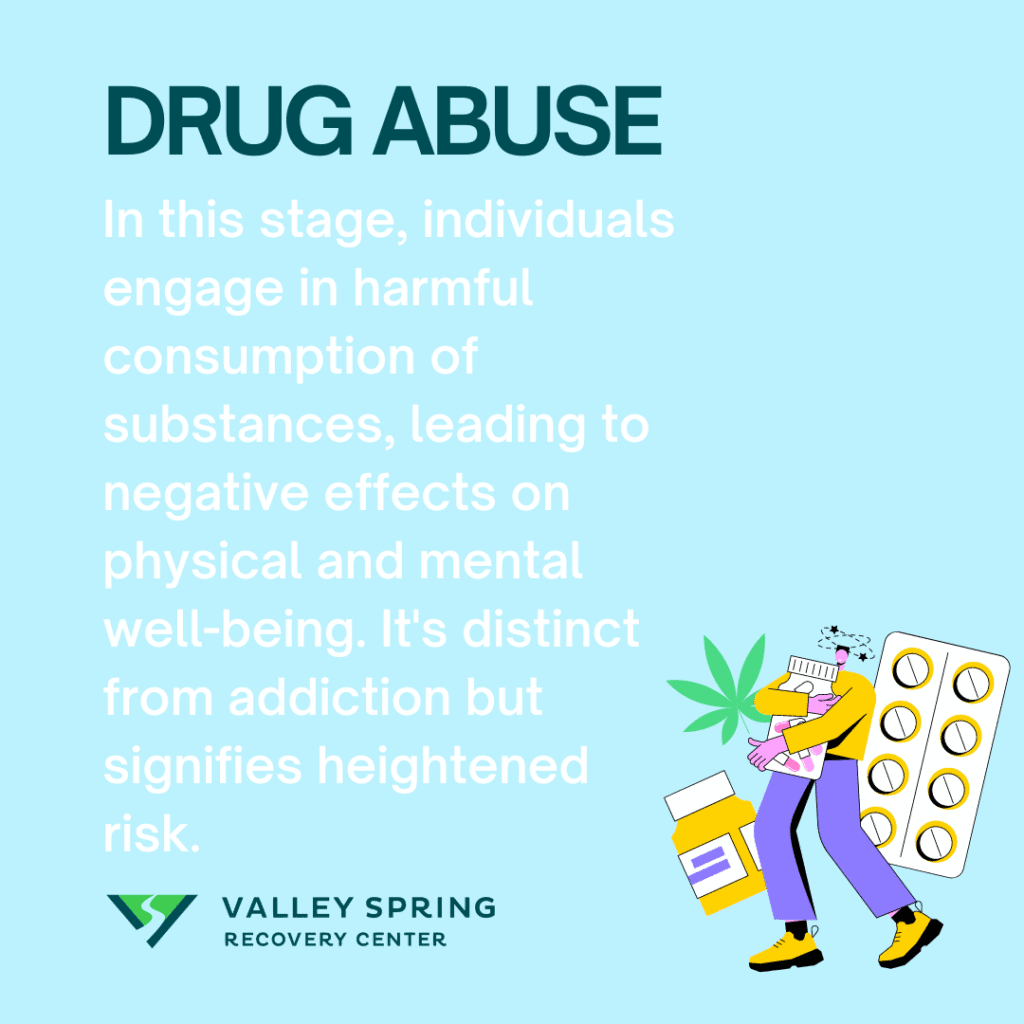
Drug abuse refers to the harmful or hazardous use of psychoactive substances, including legal and illegal drugs. Drug abuse is the second stage of the addiction cycle, where individuals engage in hazardous consumption of substances, leading to adverse effects on both mental and physical well-being, social relationships, or overall quality of life. The World Health Organization (WHO) defines substance abuse as using a substance in a harmful way.
With increased frequency and quantity of use, the risks to personal health and well-being escalate, often transitioning into drug abuse. As abuse becomes more severe, individuals are likely to develop physical and mental dependence. This dependence signifies that the body or brain has adapted to the presence of the drug, requiring increasing amounts to achieve the same effects, a phenomenon known as tolerance. The Centers for Disease Control and Prevention (CDC) report that there were over 70,000 drug overdose deaths in 2019, highlighting the severe consequences of escalating drug use (CDC, 2020).
Drug abusers have progressed past the stage of experimentation and are at heightened risk of developing physical tolerance and full-blown addiction. This stage is distinct from tolerance and dependence, as full tolerance and physical reliance have not yet manifested. For instance, problematic drinking resulting in blackouts or monthly excessive cocaine use are indicative behaviors.
According to the American Society of Addiction Medicine, people who abuse drugs exhibit behaviors like:
- Using drugs in larger amounts or for longer periods than intended
- Craving or a strong desire to use drugs
- Continued drug use despite knowing it causes or worsens a physical, social, or psychological problem
- Taking drugs to relieve or avoid withdrawal symptoms
- Increasing doses of the drug over time
Drug abuse is different from active drug addiction. While both terms are related, they’re two distinct concepts, each representing a different stage or level of drug involvement.
Drug abuse refers to a pattern of behaviors where an individual uses drugs in a way that leads to negative consequences, but it may not necessarily indicate a full-blown addiction. On the other hand, drug addiction represents a more severe and chronic condition. It is characterized by compulsive and uncontrollable use of drugs, often to the detriment of your health, relationships, and overall well-being.
What Are The Symptoms Of Drug Abuse?
The symptoms of drug abuse can vary, according to Dr Michael Olla, depending on the specific drug, frequency, and amount of use, as well as individual factors like genetics. These symptoms can range from physical to behavioral, psychological, social, and emotional. The common sign amongst all forms of drug and alcohol abuse is using the substances in a risky way and overusing substances in a way that is more than just experimentation. It’s important to understand the intent behind drug abuse. Drug abusers are looking to change the way they feel and use increasing amounts of drugs or alcohol and are past the stage of experimentation.
The signs of drug abuse are listed below:
Risky Behavior
One of the first signs of drug abuse is engaging in risky behaviors while under the influence. This may include driving, operating heavy machinery, or participating in unsafe sexual activities. Unlike experimentation, where usage might be controlled and less frequent, risky abuse often occurs more consistently but has still not progressed to physical dependence.
Overuse
Overuse of a substance is another telling symptom of drug abuse. This entails consuming larger amounts of the drug than initially intended or using the drug for extended periods. Experimentation typically involves a ‘trial’ phase, but abuse transcends this by making the drug a regular or necessary part of one’s routine.
Blacking Out
Experiencing blackouts or memory lapses is a severe symptom of drug abuse. This is rarely, if ever, an outcome of mere experimentation. Blacking out can lead to dangerous situations and is a sign that drug use has escalated to a problematic level.
Emergency Room Visits
Repeated visits to the emergency room due to drug-related complications are a glaring red flag for drug abuse. Whether it’s an overdose, an accident while under the influence, or another health crisis, frequent ER trips highlight the urgency to address the drug abuse issue.
Psychological Changes
Major shifts in mood, behavior, or psychological well-being may indicate drug abuse. This could manifest as increased anxiety, depression, or irritability. While experimentation might not significantly impact mental health, abuse often does, affecting not only the individual but also their relationships with others.
Financial Strain
Drug abuse can lead to financial difficulties, as the need to purchase the substance becomes a priority. This is generally not the case with experimentation, where the financial impact is minimal.
Neglected Responsibilities
If work, school, or home duties are consistently ignored or poorly performed due to drug use, this is a symptom of abuse. Unlike experimentation, the neglect of responsibilities shows that drug use has escalated to a disruptive level.
3. Dependence
Dependence, in the context of substance use disorder, occurs when an individual becomes reliant on a substance to function normally, stemming from the neurochemical changes in the brain due to regular drug use. Unlike tolerance, where the issue is diminished effects, dependence involves both a physical and psychological compulsion to continue using the substance to avoid withdrawal symptoms and maintain normal functioning. It is important to note that dependence extends beyond mere physical reliance and often requires increasing dosages due to tolerance, further complicating the condition.
Tolerance refers to the physiological process where a person experiences a reduced effect from a drug after using it repeatedly. As the body adapts to the drug’s continuous presence, the initial dosage no longer produces the same effect, compelling an increase in dosage to achieve the desired results. This phenomenon is common with many prescription medications and substances according to Merck manual research on Tolerance and Resistance To Drugs by Shalini S. Lynch, in 2022.
Resistance is a term often confused with tolerance but specifically relates to the ability of microorganisms or tumor cells to withstand the effects of a drug that would typically be effective against them. This is most commonly observed in the fields of oncology and infectious diseases, where the effectiveness of treatment diminishes as the targeted cells develop mechanisms to counteract the drug’s effects.
After the onset of dependence, where higher doses of a substance are required to achieve the same effects, individuals often enter the stage of full-blown addiction. Addiction is characterized by compulsive drug seeking and use, despite the harmful consequences and potential risks to physical and mental health. This stage marks a critical escalation from mere physical dependence to a chronic disorder where the psychological need to use becomes predominant.
Drug dependence should not be mistaken for addiction or drug abuse, as these are different stages in the drug addiction journey. Drug dependence is the resistance of the body to the effects of drugs. It is the result of drug abuse and one of the symptoms of full-blown addiction.
The physiological aspect of drug dependence refers to the body’s physical response to a drug. It often involves changes in the body’s metabolic processes or the functioning of receptors targeted by the drug. As a result, the body becomes less responsive to the drug’s effects, leading to the need for higher doses to achieve the desired outcome. For example, opioid tolerance can develop, requiring individuals to take increasingly larger doses to alleviate pain.
The psychological aspect of drug tolerance is the adaptation of mental and behavioral responses to a drug after repeated use. Unlike physiological tolerance, which involves changes in the body’s physical processes, psychological dependence primarily involves changes in perception, subjective experiences, and your psychological response to the drug.
What is an example of drug tolerance?
Drug tolerance occurs when an individual experiences a diminished effect of a drug after its repeated use, necessitating an increased dosage to achieve the original effect. This phenomenon can happen with various substances, but it is particularly notable with alcohol and opioids. In these cases, the body’s adaptive mechanisms reduce the drug’s impact over time, which can lead to higher consumption levels as the user tries to recapture the drug’s initial effects signaling a dependence on the drug.
What is the difference between drug tolerance and drug intolerance?
Drug tolerance and drug intolerance are two distinct phenomena related to the body’s reaction to medications. Drug tolerance refers to a situation where the body’s response to a drug diminishes over time, which can compel the user to increase the dosage to achieve the same therapeutic effect. On the other hand, drug intolerance, often confused with drug sensitivity, occurs when an individual experiences adverse effects from a drug at therapeutic or even subtherapeutic doses. This intolerance is not due to an allergic reaction, which is a more severe immune response, but rather a lower threshold for the side effects of the drug.
What is dependence syndrome?
Dependence syndrome is a medical condition characterized by a set of physiological, behavioral, and cognitive phenomena in which the use of a substance or engagement in a particular behavior takes on a significantly higher priority for an individual than other behaviors that once had more value. This syndrome is marked by a strong desire to take the drug, difficulties in controlling its use, persistent use despite harmful consequences, a higher priority given to drug use than to other activities and obligations, increased tolerance, and sometimes a physical withdrawal state according to the 2019 book Dependence Syndrome published in Psychosomatic Medicine by Kurt Fritzsche, Sonia Diaz Monsalve, Axel Schweickhardt, Catherine Abbo, Frank Kuan-Yu Chen, Kim Viet Nguyen & Van Tuan Nguyen.
4. Active Drug Addiction

The American Psychiatric Association defines addiction as a complex condition, manifesting as uncontrollable substance use despite harmful consequences (APA, 2013). Individuals in this stage may find that much of their time is spent obtaining, using, and recovering from the effects of the substance. Social, occupational, and recreational activities are frequently neglected or abandoned entirely.
Neuroscientific research provides insights into the brain changes that underpin addiction, highlighting alterations in brain systems such as reward, stress, and self-control. These changes explain the intense cravings and impaired ability to resist the drug, features that are central to addiction (Volkow et al., 2016). Once addiction develops, the individual’s ability to voluntarily cease drug use becomes severely compromised, reflecting the powerful nature of these brain adaptations.
The transition from tolerance to addiction involves both neurobiological and behavioral changes, making it a particularly challenging stage to treat. Effective treatment requires comprehensive strategies that address both the biological underpinnings and the psychological aspects of the disorder. This comprehensive approach is essential for moving into the recovery phase, where sustained treatment and support are crucial for long-term success.
Active drug addiction refers to the ongoing and current state of addiction where an individual is actively using drugs or engaging in drug-seeking behaviors despite the negative consequences they experience. It implies that the person is actively consuming a substance (such as alcohol, opioids, cocaine, methamphetamine, etc.) in a way that harms their physical health, mental well-being, and overall quality of life.
Unlike drug abuse, where drug users consume prescription medications for the purpose of achieving euphoria without necessarily experiencing the damaging effects of addiction, active drug addiction is a critical stage in the addiction cycle and can have severe consequences. Its key characteristics can range from regular substance use to cravings and dependence, severe effects, loss of control, risky behavior, tolerance, social isolation, physical and mental health decline, etc.
Active drug addiction is a prevalent issue in the U.S., with more than 21 million people aged 12 or older actively addicted to drug use in 2020, according to the National Survey on Drug Use and Health (NSDUH).
What Are The Symptoms Of Active Drug Addiction?
The symptoms of active drug addiction can vary depending on the type of drug(s) being used and the severity of the addiction. Common symptoms of active drug addiction include the following:
- cravings
- compulsive drug use
- tolerance
- withdrawal symptoms
- neglecting responsibilities
- loss of interest
- social isolation
- secrecy and deception
- financial problems
- health issues
- risk-taking behaviors
- neglect of self-care
- relationship strain
- loss of control
- crises and legal issues
- physical signs
These symptoms of active drug addiction vary from person to person and depend on the specific drug(s) being used. This means that not everyone addicted to drugs will experience all these symptoms. Additionally, the severity of addiction can range from mild to severe, with some people experiencing similar consequences but with more profound effects and strain on the quality of life.
5. Recovery And Sobriety

Ongoing recovery from active drug addiction refers to the process and commitment to maintaining a healthy, substance-free lifestyle after overcoming your addiction. It encompasses the period following initial treatment and sobriety efforts and extends throughout your life.
According to the National Institute on Drug Abuse (NIDA), Recovery is a process of change through which people improve their health and wellness, live self-directed lives, and strive to reach their full potential.
Ongoing recovery from active drug addiction involves several vital aspects, such as sobriety maintenance, coping strategies, physical and mental health well-being, lifestyle changes, continued learning, relapse prevention, support systems, etc.
What Are The Signs And Symptoms Of Ongoing Sobriety and Recovery?

The signs and symptoms of ongoing sobriety include:
- abstinence
- improved physical health
- stable mental health
- regular engagement in supportive activities
- building healthy relationships
- employment and education
- positive lifestyle changes
- enhanced self-esteem
- stress management
- relapse prevention
- community involvement
- financial stability
- hope and optimism
Remember that recovery is a highly individualized process. Achieving and maintaining sobriety is a significant accomplishment, and different people may experience these signs and symptoms to varying degrees and at different stages of their recovery and sobriety from active drug addiction.
6. Relapse

Relapse means the return to drug or alcohol use after a period of abstinence or sobriety. It is common in recovery from active drug addiction and is often seen as a setback rather than a failure. Although relapse is more common in the early stages of recovery, it can happen at any stage and is a complex and multifaceted phenomenon.
Although the symptoms of relapse are similar to the symptoms of active drug addiction, these two stages of addiction are completely different. Drug addiction relapse only happens after an individual has sought treatment and is already recovering from the addiction, while active drug addiction is the result of all the earlier stages, including experimentation, drug abuse, and tolerance.
According to Research by the National Institute on Drug Abuse, relapse rates for drug and alcohol addiction typically range from 40% to 60% or even higher. It is noteworthy that relapse rates can vary depending on the specific substance. For example, substances with severe withdrawal symptoms, like opioids or alcohol, may have higher relapse rates.
When Does Someone Start Relapsing?
Relapse occurs in the absence of active treatment and can occur at any period of time if the former addict is not addressing the chronic disease of addiction. Relapse doesn’t have a fixed timeline and can happen anytime.
A research paper published by Indian J Psychiatry in February 2018, 60(Suppl 4): S473–S478, explains that aside from the timelines, some people may begin to relapse due to cognitive factors or when they experience major life stressors, become complacent about treatment, or become too confident in their ability to stay sober.
Sometimes, people may relapse when faced with social and emotional triggers and don’t get the support they need.
What Are The Early Warning Signs of Relapse?
The early warning signs of relapse can range from behavioral, psychological, emotional, and physical characteristics. They can include the following:
- increased cravings
- isolation and social withdrawal
- negative emotional changes
- loss of interest
- decreased self-care
- dishonesty
- change in routine
- romanticizing drug use
- loss of accountability
- reduced support seeking
- return to enabling or high-risk environments
- increased impulsivity
These signs may not be present in everyone who’s beginning to relapse, but they are familiar cues to look out for. It is essential to be self-aware and vigilant while recovering from active drug addiction.
What Is The Difference Between A Slip-Up And A Full-Blown Relapse?
The difference between a slip-up and a full-blown relapse is that with a slip-up, the individual has not yet developed a tolerance or physical dependence to the drug and can quickly take active steps to discontinue drug use. Slip-ups are usually brief and have limited consequences, making it easier to retrace your steps.
On the other hand, a full-blown relapse results in the resumption of active addiction behaviors, continued drug abuse, lack of awareness and denial, more severe consequences, and difficulty regaining sobriety.
Remember that relapse is not failure. It is merely a setback, and with the right help, you can maintain a wholesome recovery.
When Does A Relapse Stop And Active Addiction Start?
Determining when a relapse ends and active addiction resumes can be complex, as it varies widely among individuals based on 6 factors that influence the transition from relapse to active addiction which are listed below.
- Period of Recovery Before the Relapse: The length and stability of recovery before relapse play a crucial role. A longer, stable recovery can result in a brief relapse, whereas a shorter or less stable recovery might lead quickly back to active addiction.
- Duration of the Relapse: How long the relapse lasts is a significant indicator. A short lapse, such as using drugs on a single occasion, may not signify a return to full-blown addiction, especially if the individual seeks help immediately. Conversely, prolonged and repeated use is a strong indicator of resumed active addiction.
- Personal Circumstances: Factors such as personal stress, life events, or environmental changes can impact whether a relapse is a one-time occurrence or a slide back into regular use.
- Behaviors and Choices: The actions an individual takes following a relapse—whether they seek support from peers, counselors, or continue using—greatly influence the potential return to active addiction.
- Support Systems: Strong support systems can help curb the escalation from relapse to active addiction. Access to therapy, support groups, and a supportive personal network can play pivotal roles.
- Mental and Physical Health: An individual’s overall health can affect how quickly a relapse might spiral into active addiction. Those with untreated mental health disorders or physical issues may be more susceptible.
It is essential for individuals and their support networks to recognize early signs of relapse and intervene promptly. The goal is to prevent the relapse from evolving into active addiction by utilizing recovery tools and resources effectively. Each case will differ, making personalized approaches to recovery and relapse prevention crucial.
At What Points in the Addiction Cycle Is Treatment Needed?
Treatment and therapy can be effective at any stage in the addiction cycle, the types of treatment and effective modalities will vary based on the individual, symptoms, and stage of drug use. Addiction is a chronic, relapsing disease that necessitates continuous treatment, even during periods of maintenance or recovery.
Drug abuse refers to the misuse of substances in a way that is harmful or risky, often leading to negative consequences in various aspects of life, such as health, relationships, and work. Over time, this abuse can lead to physical and psychological dependence, making it increasingly difficult to quit without professional help. Drug abuse without physical tolerance can be treated through partial hospitalization programs that use evidence-based therapies since medical withdrawal symptoms are usually not present in the abuse category of the addiction cycle.
Dependence is another critical stage of addiction that refers to the body’s adaptation to the presence of a drug, requiring higher doses to achieve the same effects initially experienced. This escalation in dosage can further entrench the cycle of addiction, making treatment even more crucial at this stage and also necessitating medical care in order to recover. At the stage of physical dependence, drug addicts require medical care to detox from the substance, which should take place in an inpatient rehab center.
Given its chronic and relapsing nature, addiction often requires a multi-faceted treatment approach. This can range from medical interventions like detoxification and medication-assisted treatment to behavioral therapies and long-term aftercare in an outpatient setting, even once sobriety is achieved. Even in the recovery stage, ongoing maintenance treatment is essential to manage cravings, prevent relapse, and address any co-occurring mental health conditions.
What are the four C’s of addiction?
The 4 C’s of addiction provide a framework to understand the complexities of addictive behaviors and are crucial for diagnosing and treating addiction effectively. Here’s a brief overview of each component:
- Craving: This refers to the intense and uncontrollable desire for the substance or behavior that the individual is addicted to. Cravings are powerful and can dominate a person’s thoughts and actions, leading to a preoccupation with obtaining and using the substance.
- Compulsion: This is the irresistible urge to engage in addictive behavior, despite being aware of its adverse effects. Over time, what may start as voluntary behavior becomes a compulsive action due to changes in brain chemistry caused by the addiction.
- Control (Loss of): Addiction leads to a significant loss of control over the use of the substance or engagement in the behavior. This loss of control is characterized by compulsive consumption and the inability to stop despite the desire to do so.
- Consequences (Ignoring the): Despite being aware of the negative outcomes—such as damage to health, relationships, employment, and legal issues—individuals with an addiction will continue their behavior. This disregard for consequences is a hallmark of addiction.
Understanding these 4 C’s helps in recognizing the severity of addiction and is essential for developing effective treatment strategies. Professional help and rehabilitation programs often address these components to assist individuals in breaking the cycle of addiction.
What are drug cravings and when do they occur?
Drug cravings are a significant aspect of addiction, often presenting a formidable challenge for individuals attempting to overcome substance dependence. As defined by Maarefvand, Masoomeh et al. in their 2013 study published in the Iranian Journal of Psychiatry, drug craving is characterized as an intense urge or desire to continue using a substance. This urge is a fundamental element of addiction, frequently experienced by individuals dependent on substances.
Drug cravings can occur at various times and are often triggered by specific environmental cues, emotional states, or physical conditions. These triggers can include stress, exposure to drug-related paraphernalia, social settings where substances were previously used, or even during periods of withdrawal. Cravings are particularly strong in the early stages of abstinence, making this period critical for relapse prevention.
Furthermore, Maarefvand, Masoomeh et al. highlight that individuals with opiate dependence use a variety of terms to describe their personal experiences of craving, such as jonesing or kicking, indicating that the subjective feeling of craving can vary widely among individuals. This variability underscores the complexity of addressing cravings in treatment settings, as each individual may describe and experience cravings differently.
What Stage Of The Addiction Cycle Has Withdrawal Symptoms?
Withdrawal symptoms occur when an individual who has developed tolerance and dependence reduces or stops using the substance they have been consistently consuming. This can happen at any stage after the initial experimentation phase, once the body has adjusted to regular exposure to the substance. Withdrawal reflects the body’s reliance on the drug to function normally and its struggle to recalibrate after the drug is removed.
According to the National Institute on Drug Abuse (NIDA) and corroborated by the 2009 World Health Organization study on withdrawal management, withdrawal symptoms can vary significantly depending on the substance used, the level of dependency, and the duration of drug use. For instance, approximately 50% of people who use opioids heavily experience withdrawal symptoms when they reduce or discontinue use. These statistics highlight the prevalence and challenge of managing withdrawal in the recovery process.
Effective management of withdrawal is crucial for successful rehabilitation. The Substance Abuse and Mental Health Services Administration (SAMHSA) emphasizes that tailored treatment plans, which may include medications such as methadone for opioid withdrawal or benzodiazepines for alcohol withdrawal, can alleviate the physical symptoms of withdrawal and facilitate a smoother transition to sobriety. This approach underscores the importance of recognizing and addressing withdrawal symptoms promptly to improve treatment outcomes and reduce the likelihood of relapse.
Sources
-
- https://nida.nih.gov/publications/drugs-brains-behavior-science-addiction/treatment-recovery
- Maarefvand, Masoomeh et al. “Drug Craving Terminology among Opiate Dependents; A Mixed Method Study.” Iranian journal of psychiatry vol. 8,2 (2013): 97-103.
Ben Fisher
All author postsShare This Post