Addiction significantly impacts healthcare workers, especially those in emergency departments where a high percentage of visits involve patients with substance use disorders (SUDs). These patients often require intensive care and are likely to revisit the ED, adding stress and increasing the workload for healthcare staff.
Effective interventions by healthcare workers can reduce the recurrence of emergencies and improve outcomes, highlighting the need for specialized training and support for healthcare workers dealing with SUD patients.

How are Healthcare Workers Affected by Addiction?
Addiction significantly impacts healthcare workers, particularly those in emergency departments (EDs) where individuals with substance use disorders (SUDs) frequently require care. Healthcare workers face high demands due to the complex needs of these patients, who often present with various medical and psychiatric conditions stemming from or exacerbated by their substance use.
According to a 2021 study by Zhang, Xingyu et al. in The Western Journal of Emergency Medicine analyzing ED visits in the US from 2016–2017, 11.1% of all adult emergency department visits involved patients with SUDs. Several challenges characterize these visits which are listed below:
- Higher Admissions Rates: Patients with SUDs are more likely to be admitted to the hospital (adjusted odds ratio [aOR] 1.28, CI, 1.14–1.43) and intensive care units (aOR 1.40, CI, 1.05–1.85) compared to those without SUDs.
- Increased ED Revisits: There is a higher likelihood of these patients returning to the ED within 72 hours (aOR 1.32, CI, 1.09–1.61), indicating ongoing or unresolved health issues.
- Demographic and Socioeconomic Factors: The majority of these patients are non-Hispanic White and predominantly male, with specific demographic, socioeconomic, and clinical characteristics that influence their visits.
Healthcare workers who treat individuals with addiction face a variety of risks and impacts, both professionally and personally. These challenges stem from the complex nature of addiction treatment and the often difficult circumstances of their patients. The 10 effects of addiction on healthcare workers are listed below.
- Emotional and Psychological Stress: Treating patients with addiction can be emotionally taxing. Healthcare workers may experience stress, frustration, or a sense of helplessness, particularly in cases of recurrent relapse or minimal progress. This emotional burden can lead to burnout, compassion fatigue, and even secondary traumatic stress.
- Increased Risk of Violence or Aggression: Patients with severe addiction may exhibit unpredictable or aggressive behavior. This poses a safety risk to healthcare workers, who might encounter physical violence or verbal abuse in the course of their duties.
- Exposure to Infectious Diseases: Treating individuals with addiction, especially those who use intravenous drugs, increases the risk of exposure to bloodborne pathogens like HIV and Hepatitis C. This risk is exacerbated if the healthcare setting lacks proper safety protocols or if there is accidental exposure, such as needlestick injuries.
- Legal and Ethical Challenges: Healthcare professionals working with addicts often navigate complex legal and ethical dilemmas. These may include issues related to confidentiality, informed consent, and the potential need to report certain behaviors or situations to legal authorities.
- Vicarious Traumatization: Regular exposure to the traumatic experiences of patients can lead to vicarious traumatization. Healthcare workers may find themselves impacted by the stories and experiences of those they are treating, which can affect their mental health and worldview.
- Increased Workload and Stress: Managing the acute and often severe health crises that accompany SUDs, such as overdoses or infections, adds to the workload and stress of healthcare workers.
- Need for Specialized Care: Patients with SUD often require integrated care that addresses both their immediate physical health needs and their underlying substance use issues, necessitating specialized skills and resources.
- Emotional Toll: The frequent encounters with high-risk patients who may have poor prognosis can be emotionally draining, leading to burnout among healthcare workers. Continual exposure to high-stress situations and dealing with challenging patient behaviors can impact healthcare workers’ personal lives, potentially affecting their relationships, social life, and overall well-being.
- Professional Isolation: The field of addiction treatment can sometimes be isolating. Professionals might feel that their work is misunderstood or undervalued by peers in other medical specialties, leading to a sense of professional isolation or marginalization.
- Challenges in Treatment Efficacy: Addiction is a chronic, relapsing disease, and treatment can be a long, complex process with uncertain outcomes. This unpredictability can be challenging for healthcare workers, who may struggle with feelings of ineffectiveness or disappointment when treatments do not result in lasting recovery.
How Important Is the Role of Healthcare Providers in Addressing Addiction?
The role that healthcare providers fulfill regarding drug addiction is vital for the early identification and intervention of substance use disorders. According to a study published in the Journal of the American Medical Association, only about 22% of adults who struggle with addiction received treatment in the past year. This means that many people who need help with addiction are not able to get it. However, healthcare providers can play an essential role in bridging this gap by checking all patients for addiction and referring those who need help to the right services.
The emergency department provides a critical window of opportunity to connect SUD patients with treatment and referral services. Identifying and addressing SUD during ED visits can help reduce the recurrence of emergencies related to substance use and improve the overall management of these patients. Effective intervention at this stage can potentially alleviate the long-term impact on healthcare systems and improve patient outcomes.
Healthcare workers are at the frontline of addressing the ramifications of addiction, which underscores the importance of supporting them with adequate resources, training, and emotional support systems. By enhancing the care provided to SUD patients in emergency settings, healthcare workers can not only improve outcomes for these individuals but also reduce the broader strain on healthcare systems.
Healthcare providers can help prevent drug addiction by educating adolescents about the risks of substance use. A study published in the Journal of Adolescent Health found that school-based prevention programs are effective in reducing the risk of substance use in adolescents. These programs teach coping skills and promote social norms against drug use.
Healthcare providers specializing in addiction can also provide medication-assisted treatment (MAT), which has been proven to be very effective in addiction treatment. A study published in the New England Journal of Medicine found that using medication as part of treatment is much better than just taking a placebo for treating opioid addiction. This treatment involves using specific medications like methadone or buprenorphine, which help to reduce withdrawal symptoms and the urge to use drugs.
For addiction treatment to be effective, healthcare providers must take an active role in advocating for MAT (Medication-Assisted Treatment), which bridges the gap between scientific advancements and patient care. By doing so, it can become more widely available and accessible to those who need it most, saving countless lives and transforming the way we treat addiction.
What can a healthcare worker do if a colleague is an addict?
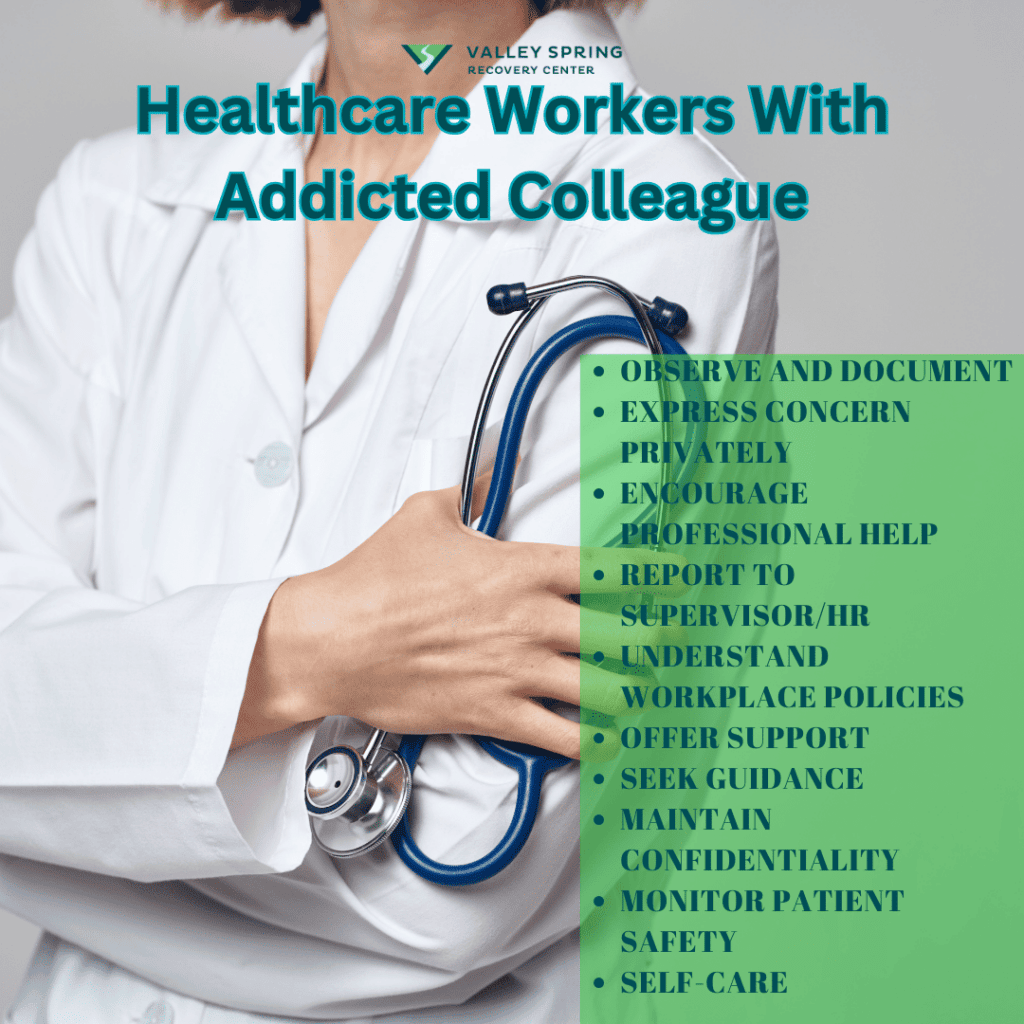
If a healthcare worker suspects that a colleague is struggling with addiction, it’s crucial to approach the situation with sensitivity and professionalism, keeping in mind both the welfare of the colleague and the safety of patients. Here are steps that can be taken:
- Observe and Document: Keep a record of specific incidents or behaviors that suggest addiction, such as frequent absenteeism, erratic behavior, changes in job performance, or physical signs of substance abuse. Documentation is important for addressing the issue effectively and responsibly.
- Express Concern Privately: If you have a good rapport with the colleague, consider expressing your concerns privately and compassionately. Approach the conversation with empathy, focusing on specific behaviors rather than making accusatory statements.
- Encourage Professional Help: Suggest that the colleague seeks professional help. This might include speaking to a mental health professional, accessing employee assistance programs (EAPs), or joining support groups for healthcare professionals dealing with addiction.
- Report to a Supervisor or Human Resources: If the colleague’s addiction is impacting their work performance or patient safety, or if they are unresponsive to informal approaches, it may be necessary to report your concerns to a supervisor or the human resources department. Ensure that this is done confidentially and respectfully.
- Familiarize Yourself with Workplace Policies: Understand your workplace’s policies regarding substance abuse and the support available for employees. This knowledge will help you handle the situation according to protocol and ensure that appropriate steps are taken.
- Provide Support and Encouragement: Offer support and encouragement to your colleague. Recovery from addiction is often a long and challenging process, and knowing that colleagues are supportive can be an important factor in successful recovery.
- Seek Guidance: If unsure about how to proceed, seek guidance from a trusted supervisor, mentor, or a mental health professional. They can provide advice on the best course of action based on the specific circumstances.
- Maintain Confidentiality: Respect the privacy and confidentiality of your colleague. Avoid gossip or sharing information with those who do not need to know.
- Monitor Patient Safety: Ensure that patient safety is not compromised. If you believe that the colleague’s condition is putting patients at risk, it’s imperative to take immediate action by informing the relevant authorities within your organization.
The effects of addiction on colleagues include extra stress, chaos and potential traumatic experiences. Ensure that you take care of your own mental and emotional health during this time.
What’s The Difference Between Addiction Psychiatry and Addiction Medicine?
The fields of addiction psychiatry and addiction medicine both deal with helping people overcome addiction, but they have some differences.
An addiction psychiatrist is a doctor who is trained to diagnose and treat not only addiction but also other mental health conditions like schizophrenia and autism. This means they have a wider range of skills to help people with addiction and other related conditions.
Addiction medicine focuses on helping people who are dealing with chronic pain caused by addiction and other health conditions like heart, lung, or liver problems. These doctors assess patients and provide treatment to help them manage their pain and improve their overall health.
What Do Addiction Doctors Treat?
Treating addiction is not an easy task. Patients who are addicted to drugs like heroin, alcohol, and other addictive substances go through a lot of discomfort during their detox period. In addition, they can continue to experience pain while undergoing rehab treatment. This is where doctors who specialize in addiction treatment come in. They must be knowledgeable about pain management solutions to help patients cope with their withdrawal symptoms. This is an important part of addiction treatment that requires specialized care and attention.
Doctors who treat people with alcohol addiction should have knowledge about the way the liver works because it’s a common issue that alcoholics face over a period of time and with prolonged consumption of alcohol.
Doctors who specialize in treating addiction have to be well-versed in the various side effects that someone going through detox may experience. They need to know which medications to use and how much to prescribe to help ease withdrawal symptoms without creating a new addiction. Doctors must have this knowledge and expertise to be certified in addiction medicine.
Doctors need to get to know their patients through individual therapy sessions. This helps them understand some of the reasons why a person may have become addicted to drugs or alcohol. By discovering which events or circumstances may have caused the addiction, doctors can better treat the problem and help patients avoid going back to it in the future.
Doctors also need to know how to treat psychological issues that can happen alongside addiction. This is all part of addiction medicine.
How Well-Trained Are Addiction Doctors?
Doctors who specialize in helping people with addiction are trained to recognize and treat the mental health problems that patients with substance use disorder often experience. These problems can include issues like depression, anxiety, post-traumatic stress disorder, and trouble sleeping.
Doctors who specialize in treating addiction are trained to understand the many different factors that can cause someone to become addicted to drugs or alcohol. These doctors need to be aware of environmental, social, hereditary, and psychological factors that can influence the development of addiction. They also need to understand how addiction can progress and what methods can be used to treat it effectively.
While addiction specialists primarily work with patients struggling with substance abuse, they are also trained to diagnose and treat behavioral addictions like gambling or food addictions.
Addiction doctors receive extensive training on the different types of therapies required for rehab treatment. This training covers individual and group therapies and the various levels of care available for addiction treatment. They also learn about different treatment settings, such as residential, outpatient, partial hospitalization, and other program types.
What Are School-Based Addiction Prevention Programs?
Preventing drug addiction is a crucial part of the national plan to reduce the number of people struggling with substance abuse. Schools play a crucial role in this effort because drug use often starts during the teenage years, and schools have many young people who can benefit from prevention programs.
Drug prevention programs employ various approaches to reduce the chances of young people getting involved with drugs. These programs seek to decrease the influence of factors that increase the risk of drug use, such as impulsive behavior or peers who use drugs. At the same time, they aim to strengthen protective factors, such as social connections and self-confidence. The main goal of school-based drug prevention programs is to prevent or delay the start of substance use among students.
In school-based drug prevention programs, trained facilitators or healthcare professionals work with students to help them stay away from drugs. These professionals are responsible for teaching students about the dangers of drugs, leading fun and interactive activities to help them remember what they’ve learned, managing classroom behavior, and involving parents and community members as needed. They ensure that the program is carried out according to plan and everyone stays safe.
How Can You Get In Touch With A Healthcare Professional Specializing in Addiction Treatment?
There are various ways to connect with addiction treatment specialists in the healthcare field.
- You can start by talking to your regular doctor. Just ask them for a referral to a specialist who can help you. They’ll be able to give you a list of qualified professionals in your area who can assist you with your recovery.
- Reach out to your local health department or mental health center. These places offer specialized services to help overcome addiction or can connect you with the right resources to get the support you need.
- Explore online databases of addiction treatment providers. These websites can help you find addiction treatment centers near you based on your needs and preferences. Some commonly used directories are:
- SAMHSA’s Find Help and Treatment portal: https://www.samhsa.gov/find-help
- The Substance Abuse and Mental Health Services Administration (SAMHSA): https://www.samhsa.gov/
- The National Institute on Drug Abuse (NIDA): https://nida.nih.gov/nidamed-medical-health-professionals
- Contact your insurance company if you need help with addiction treatment. They can provide you with a list of treatment providers covered under your insurance plan.
What Should I Consider When Selecting a Healthcare Provider for Addiction?
Once you have a list of potential service providers, it’s essential to take some time to do your research and find the one that best fits your needs. Here are some things you should consider when making your decision:
- Ensure that they are qualified to help. This means checking that they have a license to practice and that they have experience specifically treating addiction. This will help ensure you or your loved one receives the best care.
- Different providers offer different types of treatment for people dealing with addiction. There are two main types of treatment: outpatient and inpatient. Outpatient treatment means you can stay at home and attend treatment sessions during the day or evening. Inpatient treatment means you will stay at a treatment facility for a period of time to receive care and support.
- The price of getting help for addiction can be high, but there are ways to make it more affordable. Some treatment providers offer a sliding scale payment system, which means the cost is based on how much you earn. You could also get financial assistance for addiction treatment from your insurance company or a government program.
- When choosing a service provider, it’s important to consider how comfortable you feel with them and whether or not you trust them. It’s essential to select a provider who makes you feel at ease and who you can rely on.
What Are The Different Types of Addiction Treatment?
- Outpatient rehab: Outpatient rehab is a treatment option in which people receive specialized care for their addiction while still living at home. It usually involves attending a facility for no more than nine hours per week (sometimes less for teenagers), and many programs offer evening and weekend services so that people can continue to work or go to school.
- Intensive Outpatient Program (IOP): a treatment option where clients can attend therapy sessions for 10-20 hours a week (a little less for teenagers) at a specialized facility while living at home. These programs often offer evening and weekend services, so individuals can still work or attend school. IOP is a good choice for people who have medical or psychological issues that require multiple services or who have not had success with outpatient treatment.
- Partial Hospitalization Program (PHP): is a type of addiction treatment that allows clients to attend several hours of therapy a day while still living at home. Families typically use this program when their loved one needs a more intensive and structured experience. Day treatment can also be helpful for individuals who have both addiction and mental health issues.
- Inpatient rehab: When someone is struggling with addiction or a mental health issue, they might need to go to a special place to get help. This place is called ‘inpatient rehab’. It’s like a hospital but for people with addiction or mental health problems. They help people who are going through a hard time and need extra care and support.
- Medication-Assisted Treatment (MAT): If someone has a strong need for certain things like alcohol, nicotine, or opioids, they may find it difficult to quit on their own. In these cases, medicines can be helpful alongside counseling and other types of treatment.
- Alcohol Specific Rehabs: Alcohol Abuse requires intensive detox and many times residential inpatient rehab for alcoholism because the withdrawal symptoms from alcohol abuse can be severe.
Ben Fisher
All author postsShare This Post