Dual diagnosis refers to the presence of both a mental health disorder and a substance use disorder in the same individual This co-occurrence is common and affects millions of people in the United States and worldwide.
The symptoms of dual diagnosis significantly impact a person’s well-being and make it challenging to manage both conditions effectively. To understand the scope of the issue and its effects, here are some key statistics you need to know surrounding dual diagnosis.
KEY TAKEAWAYS
- SAMHSA’s 2022 National Survey on Drug Use and Health reveals that roughly 21.5 million adults in the United States have a co-occurring mental illness and substance use disorder.
- As of 2022, nearly 44% of individuals diagnosed with a mental illness in the United States reported using illicit drugs within the past year.
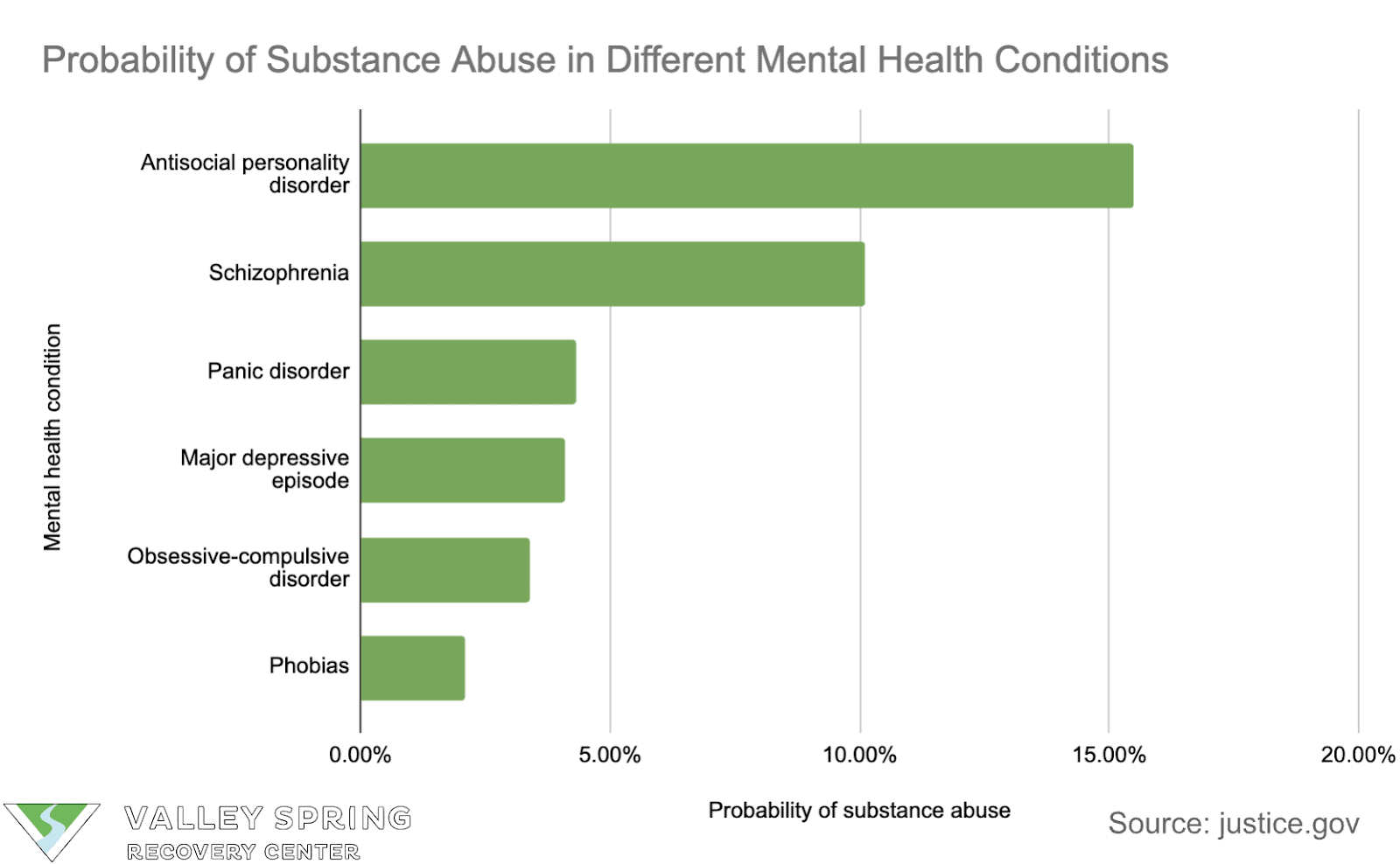
- Schizophrenia, bipolar disorder, and panic disorder are associated with a higher probability of substance abuse.
- Nearly one-third of all adults in a survey had either a substance use disorder or any mental illness within the past year, with 46% of young adults aged 18-25 experiencing either condition.
- Multiracial adults are more likely to experience both a mental illness and a substance use disorder compared to adults of other racial or ethnic groups.
- Individuals with dual diagnosis are at a higher risk of suicide and more likely to have experienced violence, property crime, and vandalism compared to the general population.
How Common Is It For Addiction And Mental Health Issues To Co Occur Together?
The prevalence of dual diagnosis in the United States is increasing, with significant impacts on healthcare due to the intertwining of mental health issues and substance abuse, exacerbated by factors like the COVID-19 pandemic.
- As per SAMHSA’s 2022 National Survey on Drug Use and Health, roughly 21.5 million adults in the United States have a dual diagnosis.
- The number of people with both severe mental illness and substance use disorder increased from 1.0% (2.3 million people) in 2015 to 1.4% (3.6 million people) in 2019.
- As of 2022, nearly 44 percent of surveyed individuals in the United States diagnosed with a mental illness stated they had used an illicit drug within the past year.
- In 2019, 7.7 million adults experienced both mental health issues and substance use disorders simultaneously.
- Among the 20.3 million adults dealing with substance use disorders in 2019, 37.9% also grappled with mental illness. Out of the 42.1 million adults experiencing mental illness, 18.2% also struggled with a substance use disorder.
- Individuals diagnosed with mental health conditions, personality disorders, or substance use disorders have a higher likelihood of turning to nonmedical use of prescription opioids.
- Commencing drug use at an early age increases the risk of developing substance use disorders later in life. Early drug use also increases the risk of experiencing mental illnesses at a later stage.
- Mental illnesses linked with persistent substance abuse include schizophrenia, bipolar disorder, manic depression, attention deficit hyperactivity disorder (ADHD), generalized anxiety disorder, obsessive-compulsive disorder, post-traumatic stress disorder, panic disorder, and antisocial personality disorder.
At Valley Spring Recovery Center, We treat mental health and substance use disorder in an integrated way that yields real results.
What Are The Dual Diagnosis Statistics Across Different Demographics?
The occurrence of dual diagnosis varies significantly across different demographic groups. Age, gender, ethnicity, and socioeconomic status all play a role in the prevalence, presentation, and access to treatment for individuals struggling with both a mental health condition and a substance use disorder.
- In 2021, 13.5% of young adults aged 18 to 25 experienced both a substance use disorder and a mental illness within the past year.
- In a survey, nearly one-third of all adults had either a substance use disorder or a mental illness within the past year.
- 46% of young adults aged 18-25 experienced either a substance use disorder or a mental illness.
- The proportion of adults aged 18 or older meeting criteria for both a mental illness and a substance use disorder within the past year was higher among multiracial adults.
- In 2021, Asian adults were less likely than adults in most other racial or ethnic groups to have experienced both Any Mental Illness (AMI) and a substance use disorder within the past year.
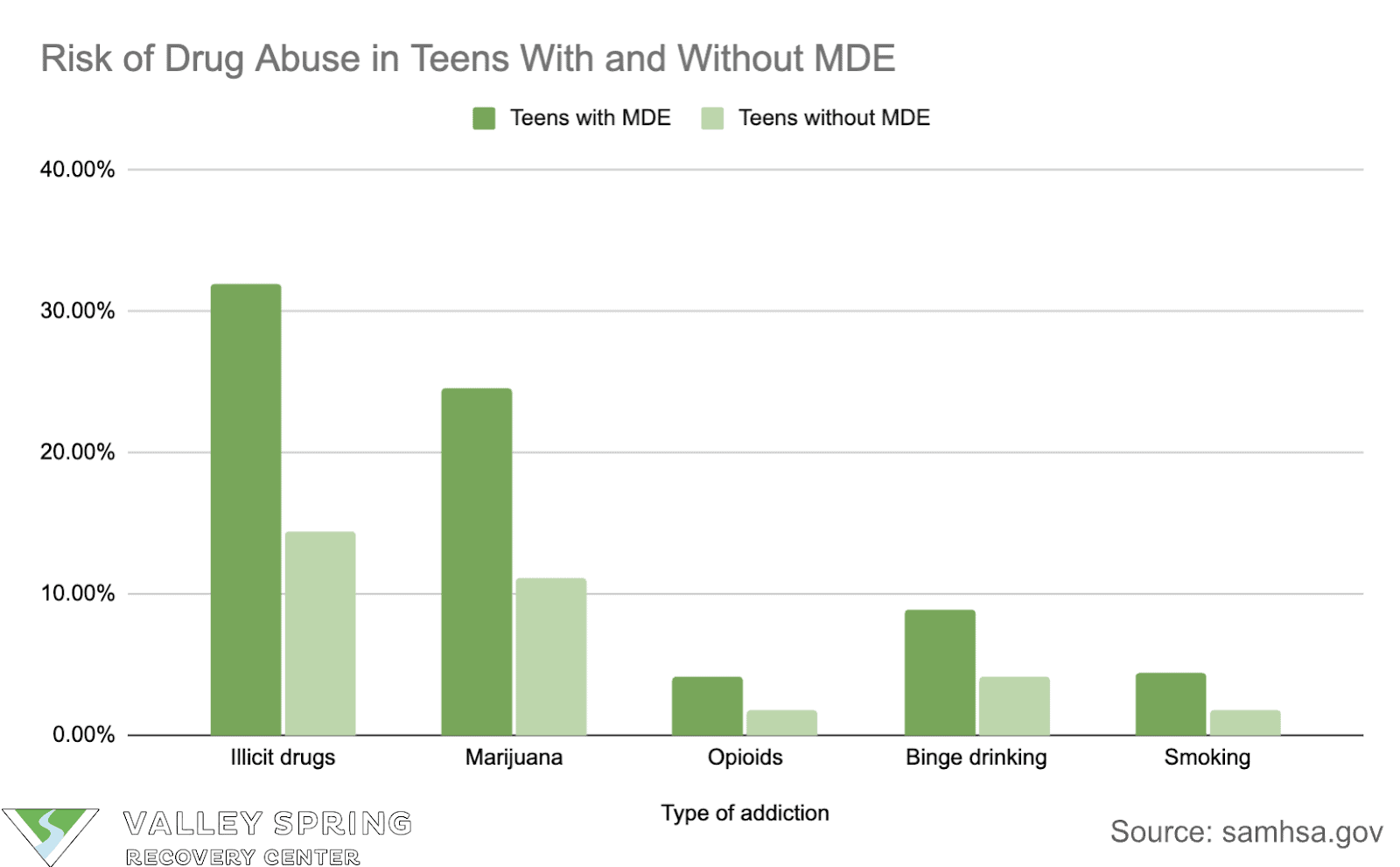
- Teens with a major depressive episode (MDE) were more likely to use drugs compared to teens without MDE between 2018 and 2019.
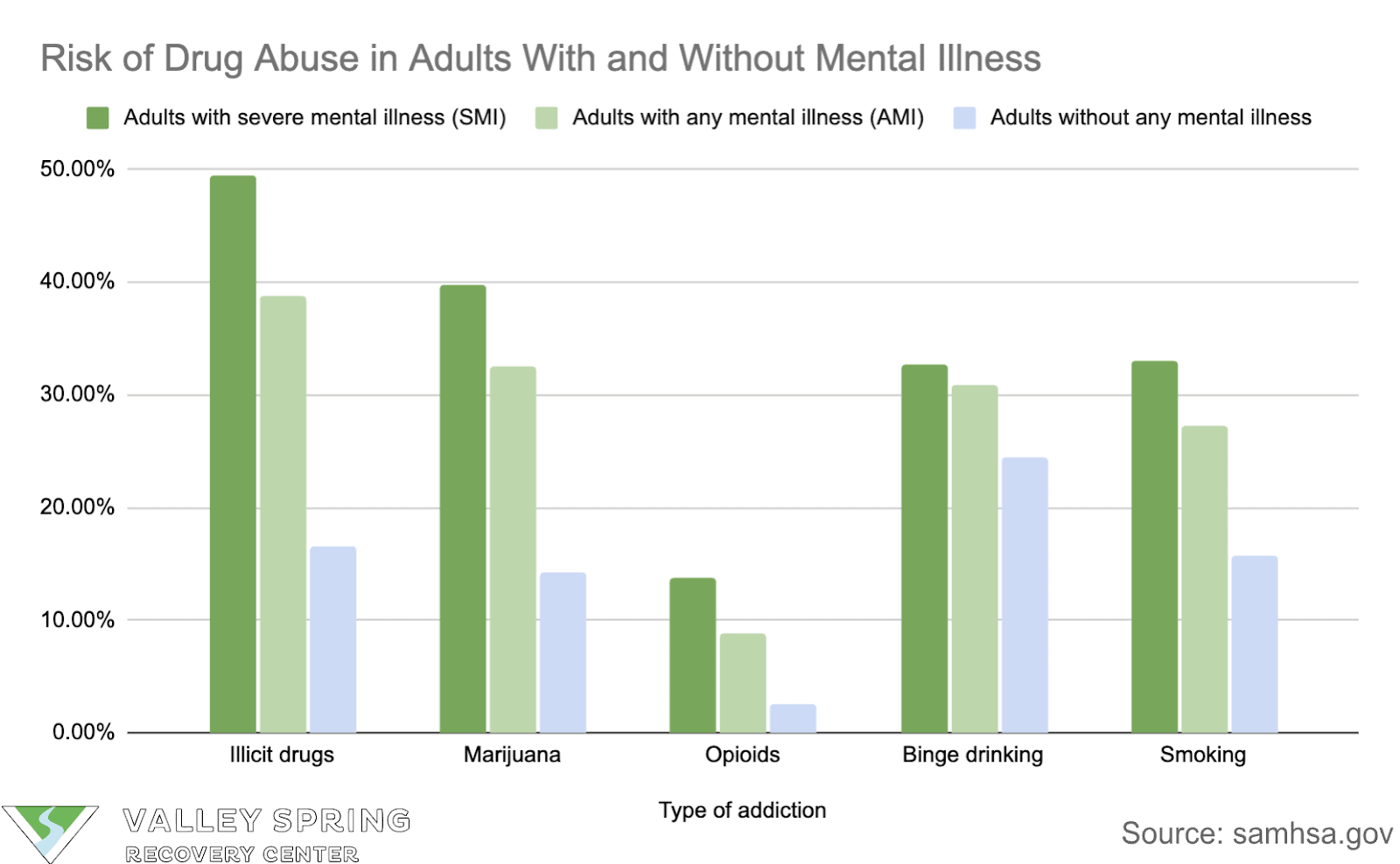
- Adults with a Serious Mental Illness (SMI) or AMI in the past year were more likely to use substances compared to adults with no mental illness.
Dual Diagnosis Treatment Statistics
Despite the high prevalence of dual diagnosis, many individuals don’t receive the integrated treatment they need. Here are some key dual diagnosis treatment statistics:
- Among the 397,000 adolescents aged 12 to 17 in 2019 who experienced both a Substance Use Disorder (SUD) and an MDE within the past year:
- 66.3%, or 263,000 individuals, received either substance use treatment at a specialty facility or mental health services within the past year.
- 62.5%, or 249,000 individuals, received only mental health services.
- 2.4%, or 10,000 individuals, received only substance use treatment at a specialty facility.
- Of the 9.5 million adults aged 18 or older in 2019 who encountered both a SUD and AMI within the previous year:
- 48.6%, or 4.6 million individuals, received either substance use treatment at a specialty facility or mental health services within the past year.
- 38.7%, or 3.7 million individuals, received only mental health services.
- 7.8%, or 742,000 individuals, received both substance use treatment at a specialty facility and mental health services.
- Out of the 3.6 million adults aged 18 or older in 2019 who suffered from both a SUD and SMI during the previous year:
- 66.6%, or 2.4 million individuals, received either substance use treatment at a specialty facility or mental health services within the past year.
- 52.0%, or 1.9 million individuals, received mental health services only.
- 12.7%, or 452,000 individuals, received both substance use treatment at a specialty facility and mental health services.
- 1.9%, or 68,000 individuals, received only substance use treatment at a specialty facility.
At Valley Spring Recovery Center, We treat mental health and substance use disorder in an integrated way that yields real results.
What Are The Effects of Dual Diagnosis
- Individuals with a dual diagnosis are at a higher risk of suicide compared to those with either a mental disorder or a substance-related disorder.
- Patients with dual diagnosis are more likely to have experienced:
- Violence: 60% compared to 11% in the general population.
- Property crime: 58% compared to 30% in the general population.
- Vandalism: 21% compared to 14% in the general population.
- Threats, sexual assault, physical assault, robbery, bicycle theft, other theft, and vandalism are more frequent among patients with dual diagnosis compared to the general population.
- In many SUDs and mental health conditions, individuals struggle to regulate their behavior to handle everyday life situations, including those involving work and relationships. Compromised coping mechanisms lead to emotional breakdowns.
What Mental Health Disorder Has the Highest Rate of Substance Use Disorder?
Research suggests that individuals with antisocial personality disorder and schizophrenia have a significantly higher rate of substance use disorder compared to other mental health conditions.
Is Addiction a Mental Illness?
Yes, the Diagnostic and Statistical Manual of Mental Disorders (DSM-5-TR) considers addiction a mental illness. It’s categorized as a substance use disorder (SUD). Addiction involves uncontrolled use of a substance despite negative consequences and impacts brain function and behavior.
However, addiction is not solely a mental health issue. It’s a complex condition influenced by various factors, including biological, psychological, and social.
What Comes First, Mental Illness or Substance Abuse?
Determining whether mental illness or substance abuse comes first is difficult because it is not a direct cause-and-effect relationship.
People experiencing mental health struggles may turn to substances like alcohol or drugs to cope with difficult emotions or symptoms.
Conversely, substance abuse may trigger or worsen mental illness. The changes substance abuse causes in the brain can increase the risk of developing depression, anxiety, or even psychosis.
What are the most common dual diagnosis disorders?
The most common dual diagnosis disorders include combinations of substance use disorders with mental health conditions such as depression, anxiety disorders, bipolar disorder, and schizophrenia. These co-occurring disorders often involve the misuse of substances like alcohol, cannabis, and opioids alongside the mental health issues.
What Is the Link Between Depression and Addiction?
The link between depression and addiction is bidirectional, meaning they influence each other:
- Depression leading to addiction: Individuals struggling with depression experience symptoms like low mood, hopelessness, and loss of interest in activities. To cope with these negative emotions, they may turn to substances like alcohol or drugs to seek temporary relief.
- Addiction leading to depression: Substance abuse and addiction impact various aspects of life and cause relationship problems, financial difficulties, and health issues. These consequences can contribute to feelings of guilt, shame, and isolation, all of which are also symptoms of depression.
What are the best dual diagnosis treatment options?
Effective dual diagnosis treatment options typically involve a combination of medication management, psychotherapy, and support groups, tailored to address both the substance use disorder and the co-occurring mental health condition simultaneously. Key approaches include Cognitive Behavioral Therapy (CBT), Dialectical Behavior Therapy (DBT), integrated group therapy, and comprehensive case management to support recovery and prevent relapse.
How do mental health and addiction statistics vary by state?
The mental health statistics of each state vary different environmental and community influences can affect the mental health of a population. For instance, seasonal depression, health insurance, access to support all have an impact on the different mental health statistics of a state and county. The New Jersey mental health statistics showed 14.6% of adults suffer from depressive episodes reported to their primary physician.
Where to get dual diagnosis treatment?
Dual diagnosis treatment is available at substance use disorder rehabilitation programs throughout the country that also have specialized staff to meet the needs of individuals with mental health conditions. Valley Spring Recovery Center has a dual diagnosis program in New Jersey with admissions counselors standing by 24/7 to meet the needs of individuals and families seeking treatment for loved ones.
Dr. Michael Olla
All author postsShare This Post