Catatonia: What It Is, Warning Signs, Causes, and Treatment Approaches
Catatonia is a serious neuropsychiatric condition marked by abnormal motor behavior, speech disturbances, and reduced responsiveness. It’s not a standalone disorder but occurs with conditions like schizophrenia, bipolar disorder, major depression, or medical illnesses. A study by Rogers et al. reports an incidence of 10.6 episodes per 100,000 person-years, though New Jersey-specific data is limited.
Common symptoms include stupor, mutism, waxy flexibility, posturing, echolalia, echopraxia, agitation, negativism, grimacing, and purposeless movements. Individuals may switch between immobility and agitation, and without treatment, basic functions like eating and hygiene may be affected.
Catatonia assessment tools like the Bush-Francis Catatonia Rating Scale (BFCRS) help clinicians identify and evaluate the severity of symptoms. Other tools include the Northoff Scale and DSM-5 criteria.
Catatonia treatment focuses on relieving symptoms quickly and addressing the root cause. Benzodiazepines, especially lorazepam, are the first-line treatment. If ineffective, electroconvulsive therapy (ECT) is highly effective. Supportive care, hydration, nutrition, and monitoring are vital during recovery.
What is Catatonia?
Catatonia is a neuropsychiatric syndrome characterised by abnormal movement, behaviour, and speech associated with mental illnesses like mood disorders or neurological conditions such as epilepsy.
It’s not classified as a separate mental illness but as a syndrome that shows up in both psychiatric disorders, like bipolar disorder or schizophrenia, and neurological conditions such as epilepsy, stroke, or brain injury.
You might experience it as complete stillness, stiff muscles, or an inability to speak. For others, it shows up as restlessness, unusual movements, or even sudden aggression. These symptoms make it hard to function or connect with others, and they go unnoticed without proper medical attention.
There are three types of catatonia. In excited catatonia, you feel hyperactive, agitated, or out of control. With retarded catatonia, the most common type, you feel frozen—unable to move, speak, or respond. Malignant catatonia is rare but dangerous. It involves symptoms like high fever, confusion, and unstable heart rate or blood pressure, and needs emergency treatment.
Though catatonia is relatively uncommon, affecting about 5–20% of people in psychiatric care, it’s most commonly seen in those with mood disorders. If you or someone close to you shows signs of catatonia, it’s important to get medical help right away.
What are the Symptoms of Catatonia?
The symptoms of catatonia include a wide range of motor and behavioural disturbances, such as immobility, rigidity, mutism, and echolalia. These symptoms manifest in various ways, from complete lack of movement to abnormal repetitions of speech or actions.
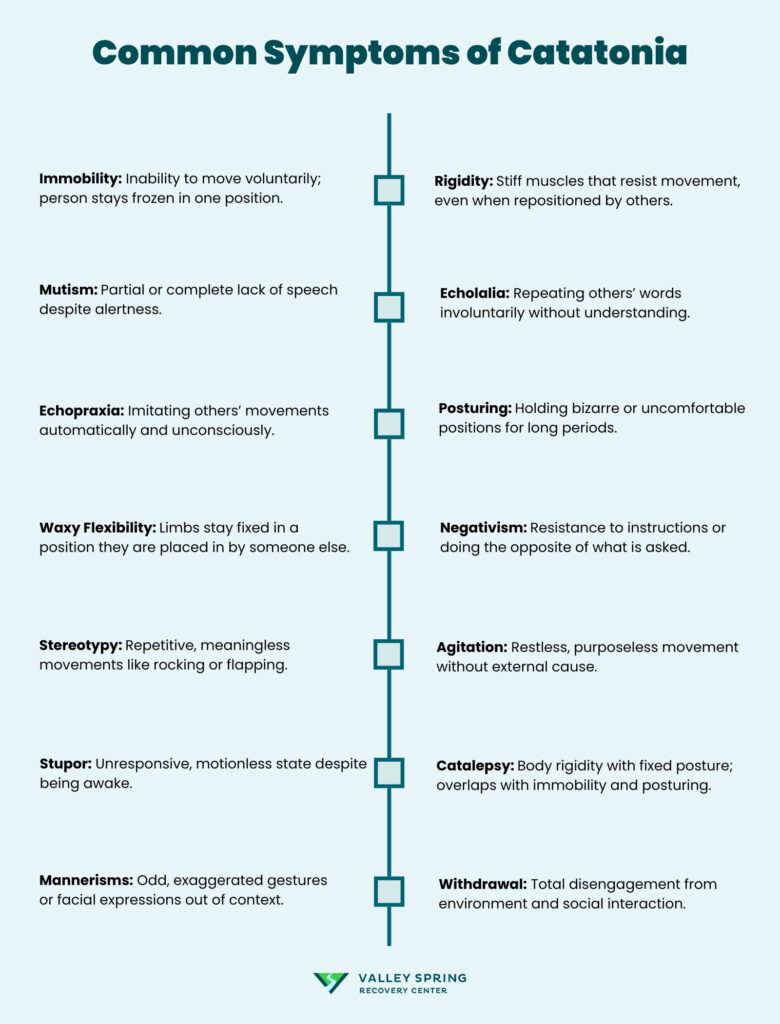
The detailed list of the most common symptoms of catatonia is as follows:
- Immobility: Immobility is the inability to move voluntarily, seen as the individual remaining frozen in a particular position for extended periods. It leads to muscle stiffness and joint pain due to prolonged stillness.
- Rigidity: Rigidity refers to stiff, inflexible muscles that resist movement, even when someone tries to adjust the person’s position. This is a motor symptom where the body is tense, and attempting to move the limbs is met with significant resistance.
- Mutism: Mutism is the complete or partial inability to speak, in which the person does not respond to questions or verbal prompts despite being conscious and alert. This symptom reflects an extreme withdrawal or shutdown of verbal communication.
- Echolalia: Echolalia is the involuntary repetition of words or phrases spoken by others. It’s a behavioural symptom in which the individual mimics or echoes what they hear without understanding the meaning or context of the words.
- Echopraxia: Echopraxia involves imitating the movements or gestures of others without intent. Individuals with this symptom mirror actions like waving or tapping in an automatic, unconscious manner.
- Posturing: Posturing refers to the individual holding awkward or unusual body positions for long durations. These positions are uncomfortable and held without regard to external stimuli or the environment.
- Waxy Flexibility: Waxy flexibility occurs when a person’s limbs remain in whatever position they are placed, even if it’s unnatural or uncomfortable. This rigidity allows their limbs to be moved by others but remains fixed in place once positioned.
- Negativism: Negativism involves resistance to external stimuli or instructions. A person refuses to move or perform an action even when asked, and in some cases, the person does the opposite of what is requested.
- Stupor: Stupor is a state of near-unconsciousness or deep lethargy where the individual appears awake but is unresponsive to their surroundings. In this state, they do not react to pain, touch, or verbal prompts.
- Agitation: Agitation in catatonia is marked by excessive motor activity that seems to have no purpose or goal. The person paces, fidgets, or displays restlessness without responding to external requests to calm down.
- Stereotypy: Stereotypy refers to repetitive, purposeless movements or behaviours, such as hand-flapping or rocking. These actions are performed in a fixed, repetitive manner without clear motivation or cause.
- Catalepsy: Catalepsy is a condition where the body becomes rigid and unresponsive, holding an awkward posture for extended periods. This symptom is a hallmark of catatonia and usually overlaps with immobility and posturing.
- Mannerisms: Mannerisms are exaggerated, bizarre movements that appear out of context, like odd gestures or peculiar facial expressions. These are voluntary actions that are abnormal in their intensity or repetition.
- Withdrawal: Withdrawal refers to the person’s complete disconnection from their surroundings, including a lack of social interaction, communication, or engagement with the environment. This symptom is a sign of severe mental disengagement.
What Causes Catatonia?
The causes of catatonia include bipolar disorder, mood disorders, schizophrenia, and autoimmune diseases. The onset of catatonia is complex and typically linked to disruptions in brain function, particularly in areas governing motor control and emotional regulation.

The causes of catatonia are as follows:
- Bipolar Disorder: Catatonia occurs during either phase, especially when mood instability reaches severe levels, leading to motor disturbances and withdrawal.
- Mood Disorders: In depressive episodes, individuals experience retarded catatonia, marked by immobility and withdrawal, while manic phases lead to excited catatonia with hyperactivity.
- Schizophrenia: Schizophrenia, a severe psychiatric disorder characterized by delusions. Catatonic schizophrenia is a subtype in which motor symptoms, such as immobility or agitation, dominate the clinical picture.
- Autoimmune Diseases: Conditions like lupus or anti-NMDA receptor encephalitis cause inflammation in the brain, leading to catatonic symptoms.
- Neurological Conditions: Damage to specific areas, like the basal ganglia or frontal cortex, is particularly linked to motor symptoms.
- Substance Use or Withdrawal: Intoxication or withdrawal interferes with brain chemistry, causing symptoms like immobility or agitation.
- Infections: Inflammation or infection of brain tissue disrupts normal motor function, leading to catatonic symptoms.
- Electrolyte Imbalances and Metabolic Disorders: Imbalances in electrolytes cause catatonia by disrupting normal brain and muscle function.
- Traumatic Events or Psychological Stress: Severe psychological trauma or stress sometimes triggers catatonic states, especially in individuals with underlying mental health vulnerabilities
Can Stress, Trauma, or Anxiety Cause Catatonia?
Yes, stress, trauma, and anxiety can cause catatonia, particularly in individuals with underlying vulnerabilities or pre-existing mental health conditions.
While catatonia is associated with psychiatric disorders like schizophrenia or mood disorders, it also emerges as a direct response to extreme psychological distress.
What Drugs or Medications Cause Catatonia?
The drugs or medications that cause catatonia include antipsychotics, benzodiazepines, opioids, and withdrawal from certain medications. These substances either trigger or exacerbate catatonic symptoms through their effects on brain chemistry, particularly involving neurotransmitters like dopamine and GABA.

The drugs and medications that cause catatonia include:
- Antipsychotics: Antipsychotics like haloperidol and risperidone alter dopamine pathways in the brain, leading to severe motor symptoms such as immobility or rigidity
- Benzodiazepines: Although benzodiazepines like lorazepam are commonly used to treat catatonia, paradoxically, their misuse or withdrawal induces catatonic states.
- Opioids: Drugs like heroin, morphine, and fentanyl depress the central nervous system and lead to catatonia, particularly when used in high doses or over prolonged periods.
- Withdrawal from medications: Withdrawal from sedatives, antidepressants, or even alcohol triggers catatonia as the brain struggles to readjust its neurotransmitter levels.
- Lithium toxicity: Lithium, a common mood stabilizer used in bipolar disorder, causes catatonia if its levels become too high in the bloodstream.
Is Catatonia a Symptom of Schizophrenia?
Yes, catatonia is a symptom of schizophrenia. Catatonia is a neuropsychiatric syndrome that affects motor and behavioral functioning, and it is recognized as one of the subtypes of schizophrenia.
The Diagnostic and Statistical Manual of Mental Disorders (DSM-5) identifies catatonia as one of the possible features of schizophrenia, alongside other psychiatric conditions.
How is Catatonia Diagnosed in New Jersey?
Catatonia is diagnosed in New Jersey using a combination of standardized diagnostic criteria, physical examinations, and psychological assessments.
The following methods are used to diagnose catatonia:
- Standard diagnostic criteria: The DSM-5 (Diagnostic and Statistical Manual of Mental Disorders) provides clear criteria for diagnosing catatonia, requiring the presence of at least three characteristic symptoms such as immobility, mutism, posturing, or echolalia. The Bush-Francis Catatonia Rating Scale (BFCRS), as mentioned in the “Bush-Francis Catatonia Rating Scale Training Manual and Coding Guide,” is another tool used by clinicians to systematically assess the severity of catatonic symptoms across a range of motor and behavioral domains.
- Physical examinations and psychological assessments: A comprehensive physical examination is conducted to rule out underlying medical conditions. Psychological assessments are also crucial to evaluate the presence of psychiatric disorders like schizophrenia or mood disorders that trigger catatonia.
- Differential diagnosis: It’s important to distinguish catatonia from other neurological or medical conditions, such as delirium, epilepsy, or neuroleptic malignant syndrome. This process ensures the accurate identification of catatonia and appropriate treatment.
How to Treat Catatonia?
To treat catatonia, a combination of medications, electroconvulsive therapy is used. Timely intervention, proper diagnosis, and individualised care are also required.
The following treatment options are used to manage and alleviate catatonic symptoms:
1. Medications
The most common medications used to treat catatonia are benzodiazepines and antipsychotics. Benzodiazepines, such as Ativan (lorazepam), are the first line of treatment. These drugs work by enhancing the effect of the neurotransmitter gamma-aminobutyric acid (GABA), which has a calming effect on the brain and body. This medication-assisted treatment helps to relieve the motor symptoms and agitation associated with catatonia.
Antipsychotics, especially atypical antipsychotics like risperidone or olanzapine, are also used if catatonia is linked to an underlying psychiatric condition like schizophrenia. However, caution is needed as some antipsychotics worsen catatonia.
2. Electroconvulsive Therapy (ECT)
Electroconvulsive Therapy (ECT) is a medical procedure in which controlled electric currents are passed through the brain to induce a brief seizure under anesthesia. ECT is one of the most effective treatments for severe or treatment-resistant catatonia.
It is especially used when medications are ineffective or when the catatonia is life-threatening (such as in malignant catatonia). ECT is highly effective in the treatment of catatonia, with response rates ranging from 80% to 100%, as studied by Luchini F et al., 2015.
3. Other Therapies for Catatonia
Other therapies for catatonia are as follows:
- Behavioral Therapy: Behavioral therapy plays a pivotal role in improving daily functionality, helping patients reintegrate into normal activities by gradually reducing catatonic symptoms. For individuals with substance use disorder, cognitive behavioral therapy (CBT) is beneficial after catatonia has subsided, helping them manage the strong negative emotions associated with both the catatonia and underlying addiction.
- Physical Therapy: Physical therapy focuses on restoring movement and physical functioning in catatonia to prevent complications such as muscle stiffness, contractures, and mobility limitations caused by extended periods of immobility. It supports muscle strength and flexibility, ensuring that patients regain independence.
- Psychological Support: Psychological support involves therapeutic interventions aimed at addressing mental health issues that contribute to catatonia, such as mood disorders or schizophrenia. This treatment helps in preventing relapses by stabilizing the patient’s mental state and offering coping strategies for managing stress and anxiety.
- Supportive Therapies: Supportive therapies include the provision of basic care, such as ensuring proper nutrition and hydration. Given that catatonic patients are unable to feed themselves or communicate their needs, maintaining adequate sustenance and hydration is critical for overall health and recovery.
- Long-term Management Strategies: Long-term management refers to ongoing care that includes regular medical checkups, psychological therapy, and monitoring to prevent the recurrence of catatonia. These strategies are vital for ensuring sustained recovery and addressing any potential triggers or underlying conditions that lead to future episodes.
Is Catatonia Curable?
Yes, catatonia is curable in many cases, especially with timely and appropriate treatment. Recovery from catatonia depends on several factors, including the underlying cause, early diagnosis, and individualized treatment.
Effective interventions such as medications (e.g., benzodiazepines), electroconvulsive therapy (ECT), and supportive therapies lead to remission of symptoms.
However, the potential for recurrence exists, particularly if the underlying psychiatric or medical condition, such as schizophrenia or mood disorders, is not fully managed. Long-term treatment plans and continuous monitoring help reduce the risk of recurrence and support sustained recovery.
Is Catatonia Preventable?
No, catatonia is not entirely preventable, as it is linked to underlying psychiatric or medical conditions such as schizophrenia, bipolar disorder, or neurological disorders.
However, early intervention, proper management of these conditions, and prompt treatment of catatonic symptoms significantly reduce the likelihood of severe or prolonged episodes.
Preventive measures include closely monitoring individuals with known risk factors, maintaining medication adherence, and ensuring regular psychiatric follow-ups to address any emerging signs of catatonia before they worsen.
How Long Does Catatonia Last?
Catatonia lasts for a few hours to several months, depending on the type and treatment. Acute catatonia lasts from a few hours to several days, especially with prompt interventions such as benzodiazepines or electroconvulsive therapy (ECT).
Chronic catatonia, however, persists for weeks or even months if left untreated or if the underlying condition is not managed.
In some cases, catatonia becomes recurrent or prolonged, particularly in individuals with psychiatric conditions like schizophrenia or bipolar disorder. Early treatment significantly shortens the duration of catatonic episodes.
How Do I Live With Catatonia?
You can live with catatonia by adopting strategies for managing catatonia symptoms and maintaining safety in daily life.
Following a treatment plan that includes prescribed medications such as benzodiazepines and therapies like Cognitive Behavioral Therapy or Electroconvulsive Therapy is necessary for preventing or reducing episodes.
Establishing a support network of family, friends, or caregivers who understand the condition and assist during episodes of immobility or rigidity is also important. Creating a consistent daily routine that focuses on self-care, nutrition, and sleep helps stabilize mood and prevent triggers.
Regular physical therapy helps maintain mobility and prevents muscle stiffness or complications from prolonged immobility, while ongoing psychological support is necessary to manage underlying psychiatric conditions like schizophrenia, bipolar disorder, or depression, which are linked to catatonic episodes.
Have an emergency plan for severe episodes and quick access to medical professionals. Minimizing stress is key, as it worsens symptoms, so relaxation techniques, mindfulness, or yoga are beneficial in managing stress levels and preventing episodes.
How to Help Someone With Catatonia?
To help someone with catatonia, it’s important to offer both physical and emotional support while being attentive to their specific needs. Start by ensuring their physical safety, especially during episodes of immobility or rigidity, as they are unable to care for themselves.
This includes helping with basic tasks like eating, drinking, and maintaining hygiene, as individuals with catatonia are unable to perform these activities independently. Recognize the importance of providing a calm, supportive environment that reduces stress, which is a trigger for episodes.
Share This Post













