The effectiveness of drug rehab is a complex question that concerns individuals battling addiction, their families, and healthcare providers. Rehab programs provide structured environments designed to help individuals address and manage their substance dependencies. However, the success of these programs varies significantly and depends on a multitude of factors including the type and severity of the addiction, the methodologies employed by the rehab facility, and the individual’s commitment to recovery.
According to the National Institute on Drug Abuse, the success rates for drug rehab programs can vary, with 40-60% of individuals maintain sobriety after treatment according to National Institute on Drug Abuse. Success in rehab is not solely measured by sobriety but also by improved quality of life and reduced relapse rates, highlighting the multifaceted nature of recovery.
Research indicates that comprehensive treatment approaches that are adaptable to an individual’s specific needs, and that provide ongoing support, significantly enhance the likelihood of a positive outcome. Effective rehab programs are characterized by their ability to adapt to the evolving needs of the patient, suggesting that a one-size-fits-all approach is often insufficient according to studies from the American Addiction Centers. This approach not only aids in immediate recovery but also bolsters long-term management of addiction, emphasizing the importance of continuous care and support networks.
The inquiry into the effectiveness of drug rehab is not just about determining if rehab works, but understanding how and when it works best. This involves acknowledging the complexity of addiction as a chronic disease and the necessity for ongoing research and refined treatment methods to enhance the efficacy of rehabilitation programs.
What is the Standard Rehab Success Rate?
The success rate of addiction treatment varies significantly depending on the type of addiction and the treatment methods employed. Research by the National Institute on Drug Abuse indicates that about 40-60% of individuals maintain sobriety one year after completing treatment. This variability highlights the challenges and complexities inherent in treating addiction, which is influenced by factors such as the severity of the addiction, the presence of co-occurring disorders, and the patient’s engagement with the treatment program according to the 2015 release by the National Institute on Drug Abuse.
According to the National Institute on Drug Abuse, 10% of U.S. adults have experienced a drug use disorder at some point in their lives, illustrating the widespread impact of addiction. Despite the significant need for treatment, only a fraction of those in need seek help. For instance, in 2020, while approximately 40 million people required treatment for substance use disorders, only about 4 million received it 2020 NSDUH Annual National Report, SAMHSA.
The Hazelden Betty Ford Foundation reports that nearly 89% of those who complete alcohol treatment remain sober for at least the first-month post-rehab. Long-term success rates are also encouraging, with 85% to 95% of individuals reporting sustained sobriety nine months after rehab. Specific detox programs have shown a success rate of 68%, and certain states like Florida report even higher success rates, achieving approximately 70% completion according to Alcohol and Drug Rehab Success Rates, Hazelden Betty Ford Foundation.
Why is treatment not successful?
Recovery from addiction involves navigating numerous challenges, including accessibility to treatment and personal reluctance to seek help. Racial and economic disparities further complicate access to necessary care. Despite these obstacles, support systems like 12-step programs significantly enhance recovery outcomes by providing essential social support and structured recovery plans according to the Recovery Research Institute.
Relapse is a common part of the recovery journey, with rates comparable to those of other chronic diseases like asthma or hypertension. It’s crucial to recognize that relapse is not a failure but rather an indication of the need for ongoing support and possibly adjustments to treatment strategies according to the 2010 news release from the National Institutes of Health.
How Is Success In Addiction Treatment Determined and Measured?
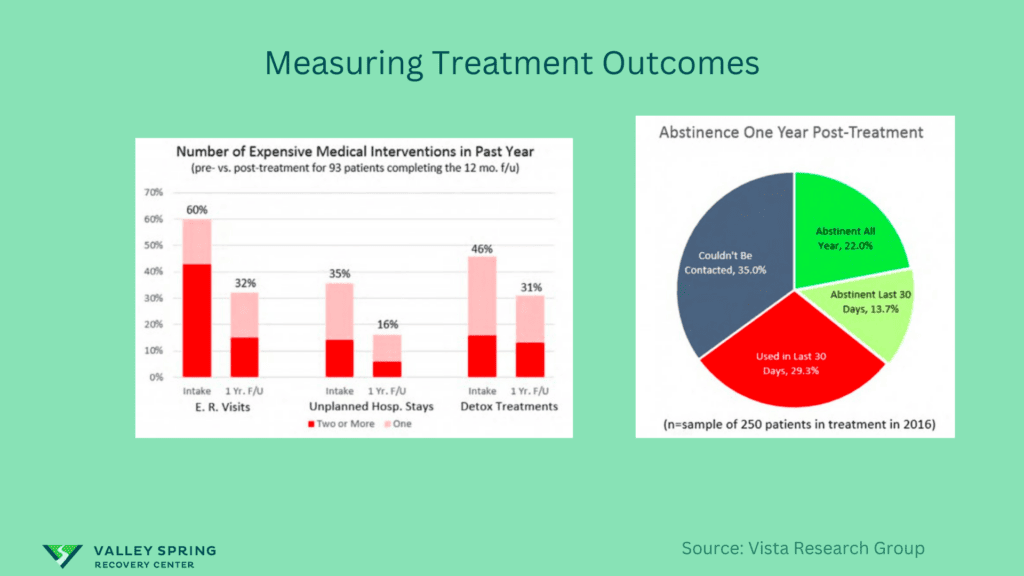
Outcomes are often measured through sobriety rates, but also through improvements in mental health, employment status, and reduced criminal activity (CDC). Vista Research Group is a company that tracks addiction treatment outcomes and success rates for rehab centers; they look at many different variables and perform follows up with patients one month, six months and twelve months after they leave treatment to learn how successful they’ve been in staying clean and sober and the impact treatment has had on their quality of life.
Is 30 Days Enough Time To Recover From Substance Use Disorder?
The effectiveness of a 30-day program also hinges on the quality of care provided. Programs that employ evidence-based practices, have a high staff-to-patient ratio, and offer personalized treatment plans are more likely to yield positive outcomes. Here are some of the factors that contribute to success or failure:
- Willingness: Recovering from chronic drug addiction is difficult and works much better if the individual is motivated and willing to follow the recommendations outlined in a treatment plan by a trained professional.
- Severity of Addiction: For those with less severe or shorter-term addictions, a 30-day program might provide sufficient initial treatment. However, for chronic or severe addiction, extended care is often recommended.
- Aftercare Planning: A 30-day program may serve as a “jump-start” for your sobriety, but long-term success typically requires continued care like outpatient treatment, therapy, and possibly sober living arrangements.
- Personal Obligations: 30-day programs are more accessible for those who cannot commit to long-term treatment due to work, school, or family obligations.
- Financial Constraints: Short-term programs are generally less expensive than long-term options, making them more accessible to some individuals. However, if the level of care is not adequate for your needs, it may not be cost-effective in the long run.
Ultimately, a 30-day program is often viewed as a starting point in the recovery process. It can be immensely valuable for detoxification, stabilization, and laying the groundwork for long-term recovery. However, addiction is generally considered a chronic disease, requiring ongoing care and lifestyle adjustments.
If you’re considering a 30-day rehab program, it’s crucial to view it as part of a more extended continuum of care. Most addiction experts recommend a follow-up treatment, including longer inpatient stays, outpatient treatment, ongoing therapy, and participation in support groups like AA or NA.
In summary, while a 30-day program can be effective under the right circumstances, it is most beneficial when considered as part of a long-term treatment strategy.
How Does Relapse Affect Drug Rehab Effectiveness?
Relapse is common and should not be viewed as a failure but rather as a sign that treatment needs to be adjusted. Approximately 50% of individuals experience at least one relapse post-treatment (SAMHSA).
Is inpatient Our Outpatient Rehab More Successful?
When it comes to drug rehabilitation, one of the first crucial decisions you’ll face is choosing between inpatient and outpatient treatment. This choice can significantly affect the course and quality of your recovery journey.
What Constitutes Inpatient Rehab?
Inpatient rehab is an immersive treatment experience where patients live in a controlled environment for a specific period, often ranging from 28 days to several months. This approach allows individuals to detach from their daily lives and stressors, providing them an isolated space to focus solely on recovery. Inpatient programs typically offer comprehensive services, including detoxification, counseling, group therapy, and medication-assisted treatments. The treatment is intensive, and staff are available 24/7 for support and medical emergencies.
What Is Outpatient Rehab?
In contrast, outpatient rehab allows patients to continue with their daily activities like work, school, and family obligations while undergoing treatment. Programs range from day treatments, which can be as rigorous as inpatient care but are conducted in a less restrictive environment, to more flexible schedules that only require attendance for a few hours per week. Though it offers freedom, outpatient care demands a higher level of self-discipline and doesn’t provide round-the-clock support.
What Is The Difference In Success Of Inpatient vs Outpatient Rehab?
The success rates of inpatient rehab vs outpatient rehab are hard to define because inpatient treatment addresses addiction at a different stage in the addiction cycle than outpatient rehab. Inpatient rehab treats individuals that are in active addiction and have physical tolerance to drugs and alcohol whereas outpatient treatment is reserved for individuals who are no longer using and have symptoms that are more mild. Here are some of the differentiating factors:
- Severity of Addiction: Inpatient care is generally better suited for individuals grappling with severe or long-term addiction, multiple relapses, or co-occurring mental health conditions. Outpatient care often works well for those with mild to moderate addiction levels.
- Personal Obligations: If you have work, school, or family commitments that you cannot leave for an extended period, outpatient treatment may be more aligned with your lifestyle.
- Support System: A strong personal support network can supplement outpatient treatment effectively. Conversely, if you lack such a network or live in an environment contributing to your addiction, inpatient care can be invaluable.
- Financial Considerations: Inpatient treatment is generally more expensive due to residential care, 24/7 support, and comprehensive services. Insurance may cover some of these costs, but this varies by policy and provider.
- Self-Discipline and Commitment: Outpatient rehab relies heavily on the patient’s commitment to adhere to the treatment plan. If you believe that you may struggle with maintaining the necessary level of self-discipline, inpatient care might be the more prudent option.
The choice between inpatient and outpatient rehab should not be made lightly. Consider factors such as the severity of your addiction, your lifestyle obligations, available support networks, and financial capacity. Consult professionals to assess your specific situation and to develop a tailored treatment plan that aligns with your recovery goals.
Understanding the distinct advantages and limitations of each modality allows you to make an informed decision, thereby optimizing the likelihood of a successful, lasting recovery.
Does The Outpatient Treatment Model Work?
Since 2002, the annual census of specialty addiction treatment facilities in the United States has consistently identified intensive outpatient treatment programs as second in prevalence only to regular outpatient treatment for alcohol and drug use disorders. In 2011, 6,089 programs in the United States reported offering IOPs (44% of 13,720 addiction treatment programs), and IOPs served 141,964 patients—12% of the 1.2 million patients in care. (SAMSHA) After completing an inpatient rehab program, the journey to full recovery is often far from over. Outpatient treatment can act as a critical follow-up to sustain the gains made during the inpatient phase. In outpatient treatment, individuals continue to receive medical supervision, and therapies, and attend group counseling, albeit in a less restrictive setting. This allows for a smoother transition to everyday life, helping to fortify new coping mechanisms while diminishing the likelihood of relapse. Thus, while not mandatory for every individual, outpatient treatment frequently serves as a vital component of a long-term, multi-faceted recovery strategy.
Criteria for Measuring Treatment Effectiveness
Effectiveness is measured through both quantitative and qualitative data, including sobriety rates, mental health assessments, and patient testimonials (WHO).
How Many People Relapse After Completing Treatment?
Approximately 50% of individuals relapse at least once post-treatment, but this should not be seen as a failure (SAMHSA).
Relapse Rates for Addiction vs. Chronic Conditions
Relapse rates for addiction are comparable to those of other chronic conditions like diabetes and hypertension, ranging from 40-60% (JAMA).
Relapse Does Not Mean Failure
A relapse is an opportunity to reassess and adjust the treatment plan and should not be considered a failure (Psychology Today).
What Can Improve the Success Rate of Addiction Recovery?
Incorporating individual behavioral therapy and personalized treatment plans can significantly improve success rates (Harvard Medical School).
Individual Behavioral Therapy
This therapy focuses on changing harmful behaviors and thought patterns that lead to addiction (APA).
Evenings In Rehab: 12-Step Meetings
12-Step meetings provide peer support that is crucial for long-term recovery (Alcoholics Anonymous).
After Rehab, What Does Recovery Look Like?
After completing a rehab program, the journey to recovery is far from over; it’s a lifelong commitment that requires ongoing effort and support. According to addiction statistics, the relapse rate for substance abuse disorders is estimated to be between 40% and 60%. This underscores the importance of a well-planned recovery strategy post-rehab. Recovery is a lifelong process that involves continuous effort and support (NIDA).
Continuous Support: One of the most crucial elements in the recovery process is having a strong support system. This can include family, friends, and support groups like Alcoholics Anonymous or Narcotics Anonymous.
Regular Check-ins with Healthcare Providers: Regular appointments with healthcare providers, including counselors and therapists, can help monitor progress and adapt treatment plans as necessary.
Medication Management: For some individuals, medication like methadone or buprenorphine may be prescribed to manage withdrawal symptoms and cravings. Proper medication management is essential for long-term recovery.
Healthy Lifestyle Choices: Exercise, balanced nutrition, and adequate sleep can significantly impact one’s recovery. A healthy lifestyle can improve mental well-being, reducing the risk of relapse.
Employment and Activity: Engaging in meaningful activities or employment can provide a sense of purpose, which is a strong deterrent against relapse.
Coping Strategies: Learning and employing new coping strategies for stress and triggers can significantly reduce the risk of relapse. Cognitive Behavioral Therapy (CBT) is often used to teach these skills.
What Are The Heroin and Opioid Use Disorder Treatment Outcomes?
The treatment outcomes for heroin and opioid use disorders can vary significantly based on several factors such as the severity of the addiction, the quality of the treatment program, and the individual’s dedication to recovery. Medication-assisted treatment (MAT), which often includes medications like methadone, buprenorphine, or naltrexone, is generally considered effective. Addiction statistics indicate that MAT can reduce opioid use and opioid-related overdose deaths by approximately 50%.
Behavioral therapies like Cognitive Behavioral Therapy (CBT) are also effective, especially when combined with MAT. These therapies help individuals understand their triggers and thought patterns that lead to opioid use. While not as rigorously studied, 12-step programs like Narcotics Anonymous have also been beneficial for many individuals by providing a strong support network crucial for long-term recovery.
Key outcomes to expect from successful treatment include a significant reduction or complete cessation of substance use, lower relapse rates, and an overall improvement in the quality of life. According to addiction statistics, comprehensive treatment programs can reduce relapse rates to below 40%. Treatment outcomes for heroin and opioid use are improving with the advent of medications like Suboxone and Methadone (FDA). Successful treatment often also leads to improved employment rates, better mental health, and stronger relationships. Additionally, effective treatment can result in a reduction in criminal activity associated with drug use, which benefits not just the individual but society as a whole.
Understanding the context in which treatment occurs is also crucial. Questions like what are the co-occurring mental health disorders that may affect treatment, or how the healthcare system in the individual’s location affects access to various treatment options, can provide a more nuanced understanding of treatment outcomes. Overall, a multi-faceted treatment approach that includes MAT, behavioral therapies, and strong support systems tends to yield the most favorable outcomes.
How do Evidence-Based Addiction Therapies affect outcomes?
Therapies like Cognitive Behavioral Therapy (CBT) and Dialectical Behavior Therapy (DBT) have shown promising results (APA).
Meth Rehab Success Rates
Success rates for meth rehab are approximately 55%, but this varies depending on the treatment methods used (SAMHSA).
Other Things You May Think About When Researching Rehab Options
Consider the facility’s credentials, success rates, and patient reviews (Better Business Bureau).
How Do You Identify an Effective Treatment Facility?
Look for accredited facilities with certified healthcare providers and positive patient testimonials (Joint Commission).
Alcohol Rehab Success Rates
The success rate for alcohol rehab is around 50-60%, depending on various factors like the length of the program and the methods used (NIAAA).
Treatment and Success Rates for Cocaine Use
Success rates for cocaine use treatment are around 40-50%, but this can improve with comprehensive care (SAMHSA).
Inpatient vs. Outpatient Rehab Patient Outcomes
Inpatient rehab generally has higher success rates due to the more intensive care provided (NIDA).
Sources
- Substance Abuse and Mental Health Services Administration. BHSIS Series S-64, HHS Publication No SMA-12-4730. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2012. National Survey of Substance Abuse Treatment Services (N-SSATS): 2011. Data on Substance Abuse Treatment Facilities.
- Day Treatment Versus Inpatient Treatment: https://pubmed.ncbi.nlm.nih.gov/10172622/
- Substance Abuse Intensive Outpatient Programs: Assessing the Evidence: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4152944/#R3
- NIDA. “Treatment and Recovery.” National Institute on Drug Abuse, 9 Mar. 2023, https://nida.nih.gov/publications/drugs-brains-behavior-science-addiction/treatment-recovery Accessed 21 Sep. 2023.
-
Vafaie NKober H. Association of Drug Cues and Craving With Drug Use and Relapse: A Systematic Review and Meta-analysis. JAMA Psychiatry. 2022;79(7):641–650. doi:10.1001/jamapsychiatry.2022.1240 https://jamanetwork.com/journals/jamapsychiatry/fullarticle/2793124
Dr. Michael Olla
All author postsShare This Post