The amygdala is a small almond-sized part of the brain forming the limbic system that derives its name from almonds due to its resemblance to the nuts.
The main function of the amygdala is to process emotions. It is also heavily involved in learning, forming memories, and reward processing.
Disorders associated with the amygdala in addiction include substance use disorders, behavioral addictions, borderline personality disorder, generalized anxiety disorder, and impulse control disorders.
Treatment options for amygdala-linked addictions are medications such as selective serotonin reuptake inhibitors, psychotherapy techniques including cognitive-behavioral therapy, and neurofeedback.
What is The Amygdala?
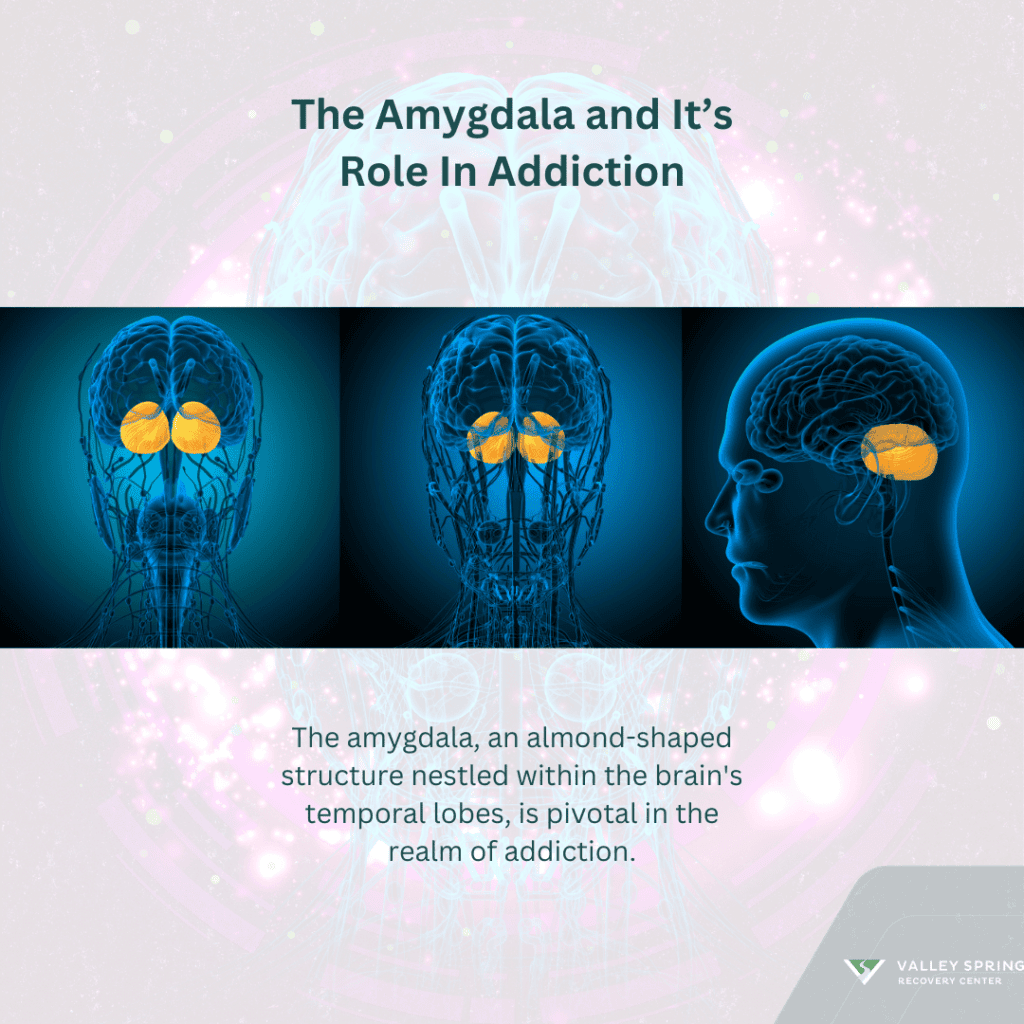
The amygdala is a small, almond-shaped structure nestled deep within the temporal lobes of the brain. It forms part of the limbic system, a network of interconnected regions crucial for emotions, memory, and motivation. The name of the amygdala is derived from its almond-like appearance and structure. It features many nuclei which are divided into five groups namely cortical-like nuclei, central nuclei, basolateral nuclei, extended Amygdala, and other amygdaloid nuclei [AbuHasan Q, et al, 2023].
This part of the brain forms part of the limbic system and is heavily involved in fearful emotions learning, emotional pleasure learning memory formation, and motivations. The amygdala’s ability to process emotions including fear, and pleasure makes it a key player in compulsive drug-seeking behavior.
What Are The Functions of The Amygdala?
The main function of the amygdala is the processing and regulation of emotions, particularly fear and anxiety. When exposed to a potential threat, sensory information is relayed to the amygdala, which rapidly evaluates the situation and initiates the appropriate emotional response. This process is crucial for survival, as it enables individuals to react swiftly to danger, triggering the “fight or flight” response.
Through intricate neural pathways, the amygdala communicates with other brain regions, such as the hypothalamus and brainstem, to orchestrate physiological responses like increased heart rate, heightened alertness, and release of stress hormones like adrenaline. Consequently, the amygdala serves as a key player in navigating threatening situations and ensuring survival, [Šimić G, et al, 2021].
The almond-shaped part of the brain plays an important role in forming and storing emotional memories. It helps encode memories associated with highly emotional events, such as traumatic experiences or intense joy, by strengthening the connections between neurons involved in the memory formation process. This phenomenon, known as emotional memory consolidation, underpins our ability to remember emotionally charged events vividly.
By controlling synaptic plasticity and long-term potentiation (LTP), the amygdala enhances the storage and retrieval of emotional memories, influencing subsequent behaviors and emotional responses. However, this mechanism can also contribute to the development of anxiety disorders or PTSD, wherein individuals experience intrusive, distressing memories linked to past traumas due to abnormal amygdala functioning.
The amygdala plays a crucial role in social and emotional learning, facilitating the recognition of facial expressions and emotional cues in others. Through its connections with regions like the prefrontal cortex and fusiform gyrus, the amygdala contributes to emotional empathy and social cognition, enabling individuals to understand and respond to the emotions of others appropriately.
Dysfunction in the amygdala can impair these social and emotional skills, leading to difficulties in interpreting facial expressions, understanding social cues, and empathizing with others, which are hallmark features of certain neuropsychiatric conditions like autism spectrum disorder (ASD).
The amygdala regulates reward processing and motivation, influencing decision-making and goal-directed behaviors. It interacts with the brain’s reward circuitry, including the nucleus accumbens and ventral tegmental area, to integrate emotional valence with motivational states, such as pleasure or aversion. By assigning emotional significance to stimuli and outcomes, the amygdala helps guide behavior toward rewarding or adaptive outcomes while avoiding potential threats or punishments. Dysregulation of amygdala function can disrupt this balance, leading to impulsive behaviors, addiction, or mood disorders characterized by deviant reward processing and motivation.
How Does the Amygdala Interact with the Brain to Influence Addiction?
The amygdala’s involvement in addiction stems from its function in processing rewarding stimuli and associative learning, [Kilts CD, 2001]. When exposed to addictive substances or behaviors, the amygdala becomes sensitized, leading to heightened activation in response to drug-related cues. This heightened reactivity contributes to the formation of strong associations between drug cues and the anticipation of reward, driving compulsive drug-seeking behaviors.
Normally, chronic drug use induces neuroplastic changes in the amygdala and its interconnected regions, leading to long-lasting alterations in reward processing and emotional regulation. These changes manifest as deficits in decision-making, impulse control, and stress responses, all of which perpetuate the cycle of addiction.
In addition, the amygdala interacts with other brain regions implicated in addiction, such as the prefrontal cortex and nucleus accumbens, forming a complex network that moderates addictive behaviors. Dysfunction within this network, driven by amygdala hyperactivity and impaired regulation, contributes to the loss of control observed in addiction.
The amygdala plays a central role in stress processing as stress is a significant factor in addiction vulnerability. Chronic stressors can dysregulate the amygdala’s stress response system, leading to increased susceptibility to addiction and heightened drug craving. This interplay between stress, the amygdala, and addiction highlights the multifaceted nature of addiction disorders.
Which Disorders Are Associated With The Amygdala in Addiction?
Disorders associated with the amygdala in addiction include substance use disorders, generalized anxiety disorder, and impulse control disorders. While the amygdala’s role in processing emotions and memories is essential for normal functioning, dysfunction in this structure contributes to:
Substance use disorders: The main disorder associated with the amygdala in addiction is substance use disorder (SUD). The amygdala plays a pivotal role in the processing of rewarding stimuli, such as drugs of abuse, by memorizing their hedonic value and reinforcing their consumption through associative learning mechanisms, [Luo, Y., 2013] . Chronic drug use leads to neuro changes within the amygdala, altering its sensitivity to reward and amplifying the salience of drug-related cues. This heightened reactivity to drug cues can trigger intense cravings and compulsive drug-seeking behaviors, contributing to the cycle of addiction.
Behavioral addictions: The amygdala plays a key role in the development of behavioral addictions such as gambling disorder and internet gaming disorder. Similar to substance addiction, behavioral addictions are characterized by dysregulated reward processing and heightened cue reactivity, both of which involve the amygdala’s dysfunction. For instance, individuals with gambling disorder exhibit hyperactivity in the amygdala in response to gambling-related cues, reflecting the salience of these cues and their ability to trigger compulsive gambling behaviors.
Post-Traumatic Stress Disorder (PTSD): PTSD is a mental health condition triggered by a terrifying event, causing flashbacks, nightmares, and severe anxiety. The amygdala’s hyperactivity in PTSD patients is well-documented. Traumatic memories associated with addiction can lead to heightened amygdala responses, intensifying cravings, and impulsive behaviors. This dysregulation contributes to the cycle of addiction, where substance use temporarily alleviates emotional distress but exacerbates long-term psychological symptoms.
Generalized Anxiety Disorder (GAD): GAD is characterized by persistent and excessive worry about various aspects of life. Studies show that individuals with GAD exhibit amygdala hyperactivity, leading to increased sensitivity to threatening stimuli. Substance dependency heightens the anxiety response and drives individuals to seek relief through substance use, perpetuating the cycle of dependence. Over time, continued substance abuse further dysregulates the amygdala’s fear response, exacerbating anxiety symptoms and fueling addictive behaviors.
Impulse Control Disorders (ICDs): ICDs encompass a range of conditions characterized by the inability to resist urges or impulses that may be harmful to oneself or others. The amygdala plays a crucial role in impulse control, modulating responses to rewarding stimuli and inhibiting impulsive behaviors. Dysfunctions in amygdalar circuitry contribute to impulsivity observed in addiction, where individuals prioritize immediate gratification over long-term consequences. This impairment in decision-making processes perpetuates addictive behaviors, leading to continued substance abuse despite adverse outcomes.
Borderline Personality Disorder (BPD): BPD is characterized by unstable moods, interpersonal relationships, and self-image, often accompanied by impulsive behaviors. Dysregulation of the amygdala’s emotional processing contributes to the intense emotional experiences observed in BPD. Individuals with BPD may use substances as a maladaptive coping mechanism to alleviate emotional distress or regulate mood fluctuations. However, chronic substance abuse further disrupts amygdala function, exacerbating emotional instability and impulsive behaviors, reinforcing the cycle of addiction.
Obsessive-Compulsive Disorder (OCD): OCD involves intrusive thoughts (obsessions) and repetitive behaviors (compulsions) performed to alleviate anxiety or prevent perceived harm. The amygdala’s involvement in fear conditioning and threat assessment is implicated in the pathophysiology of OCD. Dysfunction in amygdalar circuitry may contribute to heightened anxiety and obsessive thoughts, driving individuals to engage in compulsive rituals or substance use to alleviate distress. Addiction normally aggravates OCD symptoms by interfering with cognitive processes and exacerbating emotional dysregulation.
Major Depressive Disorder (MDD): MDD is characterized by persistent feelings of sadness, hopelessness, and loss of interest in activities. The amygdala’s role in processing negative emotions and regulating mood is disrupted in MDD. Dysregulation of amygdalar function contributes to heightened emotional reactivity and impaired stress-coping mechanisms observed in depression. Individuals with MDD may turn to substances as a means of self-medication to alleviate depressive symptoms. However, substance abuse can worsen mood disturbances and increase the risk of developing comorbid addiction.
What Are The Treatment Options For Amygdala-Linked Addictions?
Treatment approaches for amygdala-associated addiction are pharmacotherapy, psychotherapy, and neurofeedback.
Pharmacotherapy: This is one of the main treatment approaches for amygdala disorders associated with addiction. Medications targeting neurotransmitter systems implicated in addiction, such as dopamine, serotonin, and glutamate, can help restore the balance of neural activity within the amygdala and associated brain regions. For instance, drugs like selective serotonin reuptake inhibitors (SSRIs) alleviate symptoms of anxiety and depression commonly co-occurring with addiction, thereby indirectly modulating amygdala function. Similarly, medications like naltrexone or acamprosate, which target opioid and glutamate receptors, respectively, have shown efficacy in reducing cravings and preventing relapse in individuals with addiction-related amygdala dysregulation.
Psychotherapy: Talk therapy plays a vital role in addressing the psychological components of amygdala disorders linked to addiction. Cognitive-behavioral therapy (CBT), in particular, has demonstrated effectiveness in modifying maladaptive thought patterns and behaviors associated with addiction. By helping individuals recognize and challenge distorted beliefs about substance use and coping strategies, CBT can promote adaptive coping mechanisms and reduce the likelihood of relapse. Additionally, therapies like dialectical behavior therapy (DBT) and mindfulness-based interventions can enhance emotional regulation skills, which are often impaired in individuals with amygdala dysfunction.
Neurofeedback: Emerging techniques such as neurofeedback offer promising new options for treating addictions by directly modulating amygdala activity and retraining dysfunctional neural circuits, [Dehghani-Arani, F et al, 2013]. Neurofeedback involves real-time monitoring of brain activity, typically via electroencephalography (EEG), and providing feedback to individuals to help them learn self-regulation techniques. By targeting specific neural networks implicated in addiction, such as those involving the amygdala and prefrontal cortex, neurofeedback can facilitate neuroplastic changes and promote more adaptive patterns of brain function.
What are the long-term effects of untreated amygdala-linked addictions?
Untreated amygdala-linked addictions can have severe consequences on both physical and mental health, as well as overall quality of life. Some potential long-term effects include
- Increased risk of chronic health conditions such as heart disease, liver disease, and certain cancers.
- Damage to relationships, employment, and financial stability.
- Development or exacerbation of mental health disorders such as depression and anxiety.
- Legal issues related to substance abuse or addictive behaviors.
- Increased risk of overdose or other life-threatening complications.
It is important to seek addiction treatment as early as possible to minimize the risk of long-term consequences and improve the likelihood of successful recovery.
Can individuals with amygdala-linked addictions fully recover?
Yes, individuals with amygdala-linked addictions can achieve long-term recovery with the right support and treatment. Recovery is a lifelong process that requires ongoing commitment and effort, but many people can overcome addiction and lead fulfilling, productive lives. It’s essential to have realistic expectations and to be patient with oneself during the recovery journey.
What Chemicals Are Involved in Addiction?
Addiction is a complex condition, a brain disorder that is manifested by compulsive substance use despite harmful consequences. The chemicals that interact with the brain and are closely linked to addiction include:
- Dopamine: Often referred to as the “feel-good” neurotransmitter, dopamine plays a crucial role in the reward circuit of the brain. Most substances of abuse increase dopamine levels in the brain’s reward pathway, reinforcing the act of using the substance.
- Serotonin: This neurotransmitter is key to our feelings of happiness and well-being. While not all addictive substances directly increase serotonin levels, many influence its system by altering mood, which can contribute to substance use disorders.
- GABA (Gamma-Aminobutyric Acid): GABA is an inhibitory neurotransmitter that reduces neuronal excitability throughout the nervous system. Some drugs, like benzodiazepines, directly increase GABA activity, leading to a calming effect that can be addictive.
- Glutamate: As the brain’s primary excitatory neurotransmitter, glutamate is involved in cognitive functions like learning and memory. Substance abuse can disrupt glutamate homeostasis, contributing to addiction.
- Endorphins: These are the body’s natural pain relievers, which also produce a feeling of well-being. Opioids mimic endorphins, binding to opioid receptors in the brain to reduce pain and produce a euphoric feeling, leading to high addiction potential.
How can I support a loved one struggling with an addiction?
Supporting a loved one struggling with addiction can be challenging, but there are several ways you can help:
- Educate yourself about addiction and available treatment options.
- Offer emotional support and encouragement without enabling addictive behaviors.
- Encourage your loved one to seek professional help and accompany them to appointments if needed.
- Practice active listening and avoid passing judgment or criticism.
- Take care of your well-being and seek support from friends, family, or a therapist if necessary.
- Set boundaries and encourage the use of local recovery resources.
How does addiction therapy address neurochemical imbalances?
Addiction therapy can include medication-assisted treatment (MAT) to normalize brain chemistry, cognitive-behavioral therapy (CBT) to modify behavior and thought patterns, and support groups to encourage social support and coping strategies.
Can genetics influence the amygdala’s role in addiction?
Yes, genetics can significantly influence the structure and function of the amygdala, affecting an individual’s susceptibility to addiction. Genetic variations can modify how the amygdala processes emotions and responds to the rewarding effects of drugs, making some individuals with genetic predispositions prone to addictive behaviors.
Dr. Michael Olla
All author postsShare This Post