Cortisol is a hormone produced by adrenal glands that acts as the body’s primary stress hormone, is intricately involved in addiction due to its role in the ‘fight or flight’ response and its elevation during stress, which can perpetuate addictive behavior. It closely interacts with the brain’s reward system and hypothalamic-pituitary-adrenocortical (HPA) axis which makes it a key contributor to addictive behavior.
Cortisol helps the body respond to stress, including substance-induced stress. It also regulates metabolism and helps to manage blood pressure and immune functions.
Cortisol is produced in the adrenal glands alongside other hormones including adrenaline, and aldosterone.
It is released when the body detects a stressor, or low cortisol levels in your bloodstream. Stressors can be physical, emotional, environmental, or substance-induced. Addictive substances can aslo cause low cortisol levels in the body.
During detox, and rehabilitation Cortisol levels must be stabilized which can occur through medication, and therapies like meditation and mindfulness.
What Is Cortisol?
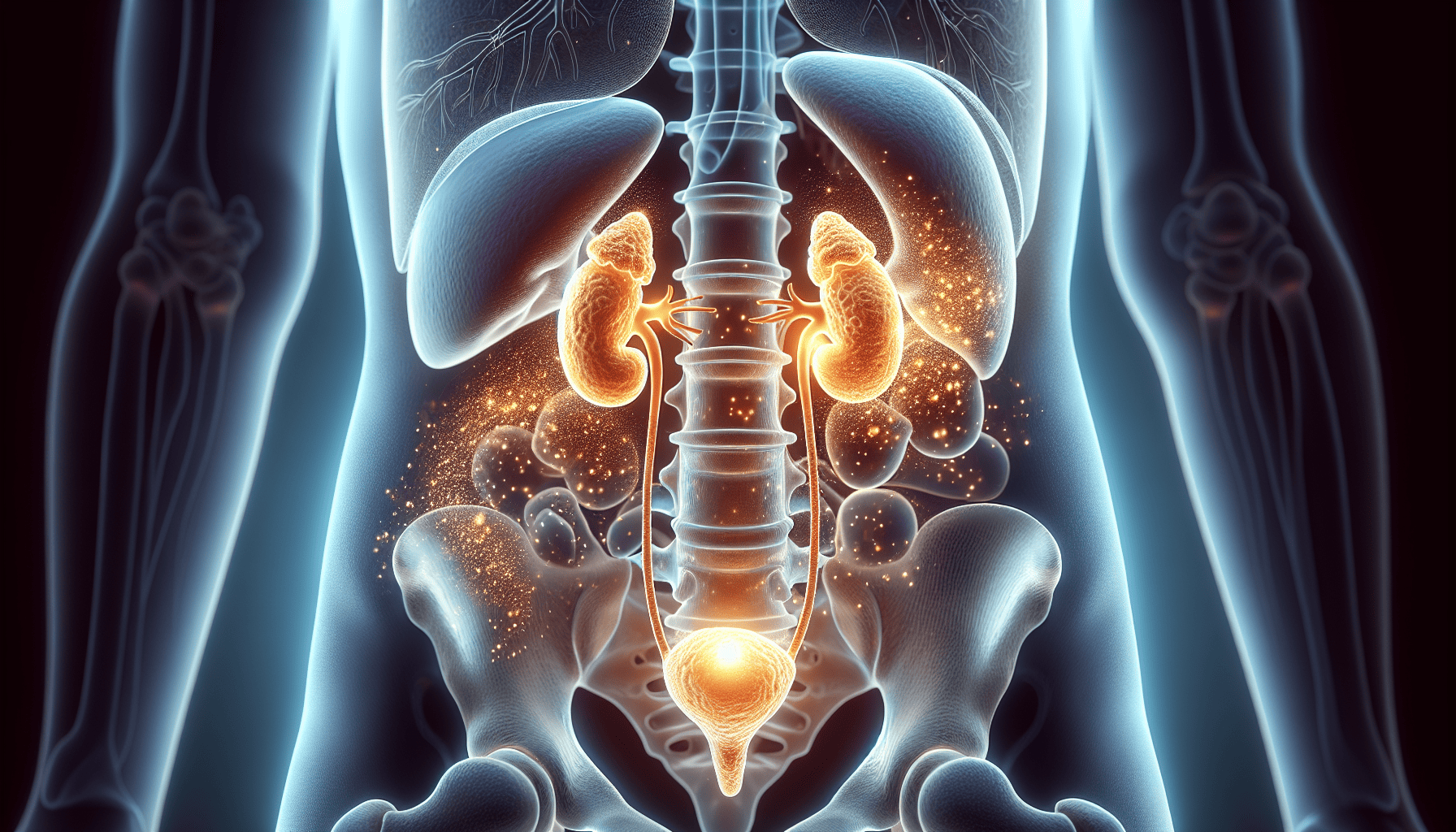
Cortisol is a steroid hormone, primarily released from the adrenal cortex’s zona fasciculata layer. This hormone circulates mostly in an inactive form, bound to either corticosteroid-binding globulin (CBG) or albumin, and is activated in most tissues. Its synthesis begins with cholesterol in the adrenal glands, and the process is initiated by the adrenocorticotropic hormone (ACTH). Adrenal glands are small glands located on top of each kidney.
Cortisol, a steroid hormone, comprises 21 carbon atoms forming a tetracyclic nucleus, including four rings: three cyclohexane and one cyclopentane. Functional groups include a ketone at position 3, a hydroxyl group at C-11, and a double bond between C-4 and C-5, crucial for its biological activity.
Cortisol belongs to a class of hormones called glucocorticoids and is involved in the breaking down of proteins, carbohydrates, and fats. In addition, they have anti-inflammatory effects.
What Is Cortisol’s role in addiction?
Cortisol interacts with the brain’s reward system, particularly the mesolimbic dopamine pathway, which is heavily involved in addiction development. The mesolimbic dopamine pathway plays a central role in reinforcement, and reward which are linked to addictive substances such as alcohol. In addition, substances such as opioids, and alcohol dysregulate cortisol levels in the brain leading to compulsion, and cravings for the drug as well as health problems including hypertension, and immune complications.
Cortisol has a significant role in addiction, being directly involved in our body’s stress response. When we experience fear or anxiety, cortisol levels rise, preparing us for the “fight or flight” response. Substance use can trigger this stress response, leading to increased cortisol levels. This rise in cortisol can intensify the addictive behavior, creating a cycle that can be hard to break.
Cortisol contributes to addictive behavior in many ways. According to a study by Lovallo, W. R. (2006) titled Cortisol Secretion Patterns in Addiction and Addiction Risk published in the International Journal of Psychophysiology, persistent intake of addictive substances such as nicotine or alcohol causes stress-like cortisol responses. Progressive use of these substances dysregulates the (HPA) axis. In addition, deficient cortisol reactivity to stressors is associated with the risk of relapse, and dependency.
The HPA is regulated by the hypothalamus using metabolic, and diurnal signals. However, when it is under acute emotional distress, its regulation is taken over by signals from the prefrontal cortex and limbic system. These changes make the HPA vulnerable to signals that reflect motivational processes driven by altered brain functions due to ingestion of substances such as alcohol, and nicotine.
Substances such as nicotine, or alcohol usually dysregulate, and destabilize the HPA axis, leading to alterations in cortisol levels and responsiveness [ Lovallo, W. R. 2006 ].
Initial Activation: The use of addictive substances often triggers a stress response in the body, leading to the release of cortisol. This initial activation of the stress response contributes to the acute effects of substance use, such as increased heart rate, heightened alertness, and temporary feelings of euphoria [Blaine, S. K. 2016].
Tolerance and Withdrawal: With continued substance abuse, the body adapts to the presence of the drug, leading to tolerance. As tolerance develops, the individual may require larger doses of the substance to achieve the desired effects. However, when the substance is no longer available, withdrawal symptoms can occur, including heightened stress and anxiety. These withdrawal symptoms are associated with dysregulated cortisol levels, as the body struggles to maintain equilibrium without the drug.
Chronic Stress: Addiction is often accompanied by chronic stress, stemming from various factors such as social, psychological, and physiological stressors. This chronic stress can perpetuate dysregulation of the HPA axis, leading to persistently elevated cortisol levels. High levels of cortisol over an extended period can have detrimental effects on physical and mental health, contributing to conditions such as anxiety, depression, cardiovascular disease, and metabolic disorders [Sinha R, 2008].
Cravings and Relapse: Cortisol plays a role in regulating motivation, reward processing, and decision-making, all of which are relevant to addiction. Dysregulated cortisol levels can influence cravings for addictive substances and impair the ability to resist relapse triggers. Additionally, stress-induced increases in cortisol may enhance the reinforcing effects of drugs, making relapse more likely.
How do The Adrenal Glands Produce Cortisol?
The adrenal glands, located at the top of our kidneys, are responsible for producing cortisol. Specifically, the zona fasciculata, the middle layer of the adrenal cortex, specializes in the production of cortisol, the main glucocorticoid hormone. The conversion process is stimulated by ACTH from the anterior pituitary, which boosts LDL receptors and cholesterol desmolase activity.
During addiction, the adrenal glands are pivotal. The increased stress response associated with substance use can overstimulate these glands, leading to an overproduction of cortisol. This surge in cortisol may intensify addictive behavior, making the conquest over addiction more arduous for individuals.
The HPA Axis: Regulating Cortisol Levels
The hypothalamus-pituitary-adrenal (HPA) axis plays a central role in modulating cortisol secretion in response to stress. Cortisol levels in our body follow a circadian rhythm, with higher levels in the morning and lower levels at night, as regulated by the HPA axis. The HPA axis is activated by the release of corticotropin-releasing hormone (CRH) from the hypothalamus, which stimulates the pituitary gland to release ACTH, in turn signaling the adrenal glands to produce cortisol.
Stress intensity, frequency, and type, whether physical or psychological, are determinants for how the PVN CRH neurons within the hypothalamus activate the HPA axis. Acute stress leads to a rapid activation of the HPA axis, triggering a quick stress response, which is typically terminated by feedback mechanisms once the stress has subsided. However, in addiction, this stress response can be continuously activated, leading to chronically high cortisol levels. This could significantly affect an individual’s health and well-being.
The Multifaceted Roles of Cortisol in Your Body About Drug Use?
Cortisol serves multiple functions in the body, going beyond its role as a stress hormone. Cortisol plays a part in:
Regulating metabolism
Regulating immune function
Mediating stress responses by mobilizing energy and ensuring resources are available to meet stress demands
Modulating the HPA axis, including the hypothalamus, pituitary, and brain structures involved in stress regulation
Regulating metabolic processes such as blood pressure, inflammation, and blood sugar levels
Playing a key role in overall metabolism
In the context of drug use, these functions can be significantly impacted. Substance use can cause a continuous activation of the stress response, leading to chronically high cortisol levels. This can disrupt the normal metabolic processes that cortisol regulates, leading to health problems such as hypertension, diabetes, and immune system dysfunction.
Metabolic Regulation and Glucose Homeostasis
Cortisol is pivotal in regulating glucose homeostasis. It stimulates the production of glucose from non-carbohydrate substrates through gluconeogenesis in the liver, involving key enzymes such as phosphoenolpyruvate carboxykinase (PEPCK). The hormone increases blood glucose levels by elevating hepatic glucose production and reducing insulin sensitivity, affecting fasting glucose concentrations and β-cell function.
These metabolic processes can be disrupted with drug usage. Chronic drug use can lead to continuous activation of the stress response, resulting in persistently high cortisol levels. This can disrupt glucose homeostasis, leading to problems such as insulin resistance and potentially contributing to the development of type 2 diabetes.
Immune Modulation and Inflammatory Response

Cortisol is also vital in modulating immune responses and inflammation. It exerts anti-inflammatory effects by inhibiting the production of pro-inflammatory cytokines and reducing the accumulation of immune cells at sites of inflammation. It regulates the immune response by suppressing the proliferation of T cells and the activity of natural killer cells, modulating both innate and adaptive immunity.
These immune and inflammatory responses can be significantly altered due to drug use. Chronic drug use can lead to a continuous activation of the stress response, resulting in persistently high cortisol levels. This can disrupt the normal immune response and lead to an overactive inflammatory response, potentially causing chronic inflammation and related health problems.
Broad Spectrum Effects: From Nervous to Reproductive Systems
The effects of cortisol extend to nearly every organ system in the body. It influences brain function by affecting mood and cognitive processes, and prolonged high levels can lead to alterations in brain structure, such as hippocampal atrophy. Cortisol also plays a role in cardiovascular health by regulating blood pressure and vascular tone, and excessive cortisol can contribute to the development of hypertension and an increased heart rate.
In the reproductive system, cortisol can influence gonadal function, and chronic stress-associated high cortisol levels can lead to disruptions in reproductive hormone balance and fertility issues such as irregular menstrual cycles in women and reduced testosterone levels in men. Furthermore, high levels of cortisol over extended periods can lead to digestive issues by influencing the gastrointestinal system, potentially causing symptoms such as heartburn or indigestion.
Cortisol at Work: Hormone Action Mechanism
Cortisol operates in our body by binding to glucocorticoid receptors. Being lipid-soluble, it can readily pass through the cellular plasma membranes and bind to these receptors, which are primarily located in the cytoplasm awaiting ligand binding. The binding of cortisol to these receptors triggers a conformational change, leading to the dissociation of associated proteins such as heat shock proteins and the translocation of the receptor into the nucleus.
Inside the nucleus, the cortisol-receptor complex binds to DNA at glucocorticoid response elements, resulting in the regulation of gene transcription, which may either stimulate or repress the expression of target genes. The diversity in glucocorticoid receptor forms through alternative splicing generates variants like GRα and GRβ, and through posttranslational modifications that influence the receptor’s transcriptional activity and stability.
How Long Does It Take Cortisol Levels To Come Back To Normal After Drug Use?
Normalizing cortisol levels post drug use can vary significantly among individuals. This is largely dependent on individual factors such as the person’s overall health, the specific drug used, and the duration and severity of the drug use.
Regular monitoring and management of cortisol levels are vital for diagnosing and treating endocrine disorders like Cushing’s syndrome and Addison’s disease. Cortisol testing must account for the hormone’s diurnal pattern, with levels peaking in the early morning, necessitating precisely timed sample collection.
Post drug use, it’s essential to manage cortisol levels to prevent these disorders and maintain overall health.
Salivary Cortisol Testing
One way to assess cortisol levels is through salivary cortisol testing. This method is convenient and non-invasive, providing a measure of free cortisol levels. Salivary cortisol tests are often conducted at night to measure the nadir of the diurnal cortisol rhythm, with elevated night-time levels being indicative of Cushing’s syndrome.
Salivary cortisol testing can serve as a useful tool for monitoring cortisol levels in relation to drug use. It can help healthcare providers assess the impact of drug use on cortisol levels and guide treatment interventions to help bring cortisol levels back to normal after drug use.
Serum Cortisol Measurements
Another method to assess cortisol levels is through serum cortisol measurements. These measurements are taken in the early morning to diagnose Addison’s disease due to the diurnal nature of cortisol secretion. An early morning cortisol level that is inappropriately low can indicate primary adrenal insufficiency.
Serum cortisol measurements can offer useful insight into the adrenal function and overall health of individuals recovering from drug use. A healthcare provider can use this information to tailor treatment interventions, helping the individual achieve normal cortisol levels and overall health.
Is Addiction Linked To Increased Cortisol Levels?
Studies have established a correlation between addiction and elevated cortisol levels. Abnormal cortisol levels can lead to serious health conditions known as hypercortisolism and hypocortisolism, commonly represented by Cushing syndrome and Addison’s disease, respectively. Cushing syndrome, or hypercortisolism, is characterized by rapid weight gain, easy bruising, and diabetes, affecting mostly individuals between the ages of 25 to 50, with a higher prevalence in women.
Addison’s disease, or hypocortisolism, can present with symptoms such as:
dehydration
severe fatigue
nausea
lightheadedness
These symptoms indicate that cortisol is crucial for multiple bodily functions including electrolyte balance and energy production. Increased cortisol levels related to addiction can, therefore, lead to these serious health conditions if not properly managed.
What is The Role of Cortisol and Neurotransmitters During Detox, and Rehabilitation
Cortisol, known as the stress hormone, plays a significant role in addiction recovery. A study by the Marshall University Joan C. Edwards School of Medicine found that cortisol levels could be indicators of addiction recovery success, suggesting that managing stress and cortisol could be critical in treating addiction.
Managing cortisol levels during detoxification and rehabilitation is important to deal with withdrawal symptoms, and preempt the possibility of relapse. In addition, it prevents the development of conditions such as hypertension, cardiovascular disease, obesity, immune suppression, and mood disorders that are linked to fluctuating levels of cortisol which would complicate the process further.
Abrupt cessation of substance use leads to withdrawal symptoms due to dysregulation of cortisol levels and other neurotransmitters that impact addiction. For example, during alcohol withdrawal, there is typically an increase in cortisol levels due to the stress response triggered by the body’s attempt to adapt to the absence of alcohol. “Alcoholics who display the most severe cognitive impairments during withdrawal are those who also have the highest cortisol levels. Therefore, cortisol function seems to play a significant role in continued alcohol dependence and risk of relapse,” says Dr. Abi Rose, a psychologist and senior lecturer in the Department of Psychology at the University of Liverpool.
There are many approaches to regulating cortisol levels during rehabilitation. These include:
- Medication-assisted treatment (MAT) – Administration of medication such as buprenorphine for opioid addiction or naltrexone for alcohol dependence indirectly influences cortisol levels by reducing the stress associated with withdrawal and cravings.
- Exercise and occupational therapy (OT)– Engaging in healthy lifestyle practices and effective stress management techniques such as exercises, and occupational therapy (OT ) is essential for promoting recovery and preventing relapse in individuals with addiction. Exercising helps in improving cortisol levels naturally while OT equips the person with skills to deal with stress, pain, and other unpleasant events in their life without resorting to using substances such as opioids, alcohol or engaging in addictive behavior.
When There Is Too Much Cortisol?
Characterized by an excess of cortisol, often tumor-induced, hypercortisolism or Cushing’s syndrome presents itself. A specific form known as Cushing disease arises from a benign tumor in the pituitary gland that leads to the overproduction of ACTH and subsequent cortisol increase. Symptoms of elevated cortisol levels include:
Sudden weight gain, especially around the face, abdomen, and back
Increased bruising or purple stretch marks
Anxiety, depression, mood swings
General tiredness
Muscle weakness
Various reproductive changes
Chronic drug use can potentially lead to hypercortisolism. The continuous activation of the stress response can result in persistently high cortisol levels, leading to the symptoms and complications associated with Cushing’s syndrome. If left untreated, Cushing syndrome can result in serious health issues such as:
infections
blood clots
depression
heart attacks
cognitive challenges
high blood pressure
broken bones
diabetes
How To Deal with Low Cortisol Levels?
Insufficient cortisol production results in hypocortisolism, or Addison’s disease. This condition is usually diagnosed in a clinical setting by demonstrating low levels of cortisol, alongside high renin levels and a diminished cortisol response to ACTH stimulation. Symptoms of Addison’s disease, exacerbated by illness or injury, can include extreme fatigue, weight loss, low blood pressure, salt craving, and over time, may lead to an Addisonian crisis requiring emergency treatment.
Particularly with substances that suppress the adrenal glands in drug use, hypocortisolism can manifest. The adrenal glands may produce too little cortisol, leading to low serum cortisol levels and a lack of response to ACTH stimulation. This can cause the symptoms associated with Addison’s disease, making it crucial to monitor and manage cortisol levels in individuals recovering from drug use.
How to Maintain Healthy Cortisol Levels?

Several lifestyle modifications are involved in maintaining healthy cortisol levels. Here are some key strategies:
Build social support networks
Engage in regular physical exercise for a recommended 150-200 minutes per week
Explore hobbies and activities that bring joy and relaxation
Ensure adequate sleep
Practice stress management techniques such as journal writing, practicing positivity, mindfulness-based stress reduction, deep breathing exercises, and maintaining supportive relationships
By implementing these strategies, you can effectively reduce stress-induced cortisol spikes and maintain healthy cortisol levels.
Maintaining a nutrient-rich diet is also key to managing cortisol levels. Some foods and supplements that may help manage cortisol levels include:
Whole grains
Fruits
Vegetables
Legumes
Green tea
Foods high in prebiotics and probiotics
Fish oil
Ashwagandha
By adopting these lifestyle changes, for example, individuals recovering from drug use can help bring their cortisol levels back to normal and maintain overall health.
When to Consult Your Doctor
Medical attention is crucial if you’re experiencing symptoms related to cortisol imbalance. Symptoms such as:
chest pain
trouble breathing
weakness on one side of the body
severe headaches
sudden loss of movement, vision, or speech
These symptoms could serve as examples of complications related to high cortisol levels, putting the body on high alert.
Consulting healthcare professionals for accurate diagnosis and treatment recommendations for cortisol imbalance is also important, given their expertise in providing accurate assessments suited to individual needs. Avoid self-diagnosis or treatment based on symptoms alone, as this may lead to inaccurate conclusions and harmful self-treatment, making professional medical advice critical.
What does cortisol tell you?
Cortisol testing involves a sample of blood, urine, or saliva, and can help diagnose conditions like Cushing’s syndrome and Addison’s disease. It measures the level of the stress hormone cortisol to screen for diseases affecting the pituitary and adrenal glands.
What happens when cortisol levels are high?
When cortisol levels are high, it can lead to rapid weight gain, high blood pressure, thinning of the bones, skin changes, and muscle weakness, among other symptoms. These symptoms indicate the potential health risks associated with elevated cortisol levels.
What does cortisol do in the body?
Cortisol is an essential hormone that regulates the body’s stress response, metabolism, and the availability of substances for tissue repair. It also influences the use of glucose in the brain and bloodstream.
How is cortisol tested?
Cortisol levels are typically assessed through salivary cortisol testing and serum cortisol measurements, which can inform healthcare providers about cortisol levels and guide treatment.
How do cortisol levels change based on dopamine levels?
Cortisol and dopamine levels interact in complex ways. Typically, high cortisol, a stress hormone, may decrease dopamine, the ‘feel-good’ neurotransmitter, leading to mood changes. Conversely, increased dopamine can lower cortisol, reducing stress. This balance affects mood, motivation, and stress response.
How does cortisol affect Withdrawal Symptoms?
Cortisol levels can rise during withdrawal, contributing to the stress and discomfort experienced, making the process challenging.
Can elevated Cortisol levels increase the risk of relapse?
Elevated cortisol levels during stressful situations increase the risk of relapse for individuals in recovery from addiction.
Dr. Michael Olla
All author postsShare This Post