Chronic exposure to drugs leads to significant changes in the brain’s neurochemistry and neuroplasticity, primarily affecting neurotransmitters like dopamine, glutamate, GABA, serotonin, norepinephrine, endorphins, acetylcholine, anandamide, oxytocin, cortisol, dynorphins, neuropeptide Y (NPY), and vasopressin. These alterations disrupt the natural balance and functioning of neural circuits within key areas such as the nucleus accumbens, often referred to as the brain’s “pleasure center.” The overstimulation of this reward circuit through drug use results in an enhanced feeling of euphoria, reinforcing the drug-seeking behavior. Over time, these neuroadaptations decrease the brain’s sensitivity to natural rewards and increase the vulnerability to relapse, making it difficult for individuals to derive pleasure from anything other than the drug.
“Chronic exposure to several classes of drugs of abuse disrupts plasticity in this region, allowing drug-associated cues to engender a pathologic motivation for drug seeking. A number of alterations in glutamatergic transmission occur within the nucleus accumbens after withdrawal from chronic drug exposure. These drug-induced neuroadaptations serve as the molecular basis for relapse vulnerability.”
(Scofield et al., 2016)
Understanding the molecular basis of addiction, including the role of the nucleus accumbens and the alteration of neurotransmitter systems, is crucial for developing effective treatments. The brain’s ability to adapt and change, or neuroplasticity, while fundamental to learning and memory, also makes it susceptible to the reinforcing effects of drugs. This dual-edged nature of neuroplasticity underscores the complexity of addiction, where the pathological pursuit of drugs stems from the very mechanisms that underpin our capacity to learn and adapt. By targeting these molecular changes and leveraging our understanding of neurotransmitter imbalances and brain plasticity, researchers and clinicians aim to create more effective strategies for prevention, treatment, and recovery from addiction.
How Do Drugs Affect The Brain?
When an individual ingests a substance with addictive potential, the immediate impact is often a surge of euphoria. According to NIDA, this sensation is primarily orchestrated by the brain’s “reward circuit,” a neural pathway that releases dopamine, a neurotransmitter associated with pleasure and reinforcement. In a well-balanced brain, this dopamine-driven reward system encourages essential survival behaviors, such as nourishment intake and social bonding. However, the introduction of drugs hijacks this system, flooding the neural circuitry with dopamine and reinforcing the drug-taking behavior.
The Phenomenon of Tolerance: As the cycle of drug use persists, the brain undergoes a series of adaptations that make the euphoria or high feeling deminish over time. Specifically, the neural cells constituting the reward circuit become less responsive to dopamine surges. This phenomenon, known as “tolerance,” results in a diminished euphoric experience compared to the initial highs. (NIDA) Consequently, individuals may escalate their drug dosage in a futile attempt to recapture the original sensation of euphoria.
The Erosion of Pleasure: One of the most insidious aspects of this neural adaptation is the erosion of pleasure derived from previously enjoyable activities. As the reward circuit becomes increasingly desensitized, the individual finds less satisfaction in activities that once brought joy, such as culinary experiences, intimate relationships, or social interactions. (NIDA) This shift often propels the individual further down the spiral of addiction, as the drug becomes one of the few remaining sources of pleasure.
Cognitive and Behavioral Impairments: Long-term drug use doesn’t merely affect the reward system; it also triggers alterations in various other neural circuits responsible for a range of cognitive functions. These include but are not limited to:
- Learning Capacity: Impairment in the ability to acquire new skills or knowledge.
- Judgment: Erosion of the capability to make sound decisions.
- Decision-Making: Compromised ability to choose between alternative courses of action.
- Stress Response: Heightened sensitivity to stressors, leading to maladaptive coping strategies.
- Memory Retention: Reduced ability to store and recall information.
- Behavioral Regulation: Increased impulsivity and risk-taking behaviors.
Stopping Becomes Difficult: Despite cognizance of these detrimental outcomes, many individuals find themselves unable to discontinue drug use. This self-destructive behavior epitomizes the essence of addiction—a condition where the individual is ensnared in a cycle of substance abuse, even when aware of its harmful repercussions. This is why addiction is a chronic relapsing disease.
How Are The Brain And Neurotransmitters Involved in Drug Addiction?
Addiction involves a complex connection of neurotransmitters like dopamine and glutamate, which affect the brain’s reward system, learning, and memory, leading to reinforced drug use and cravings. Other key neurotransmitters and brain chemicals, including GABA, serotonin, norepinephrine, endorphins, acetylcholine, anandamide, oxytocin, cortisol, dynorphins, neuropeptide Y (NPY), and vasopressin, play significant roles in mood regulation, stress response, social behavior, and the overall addiction process, highlighting the multifaceted nature of addictive disorders and potential treatment targets according to NIDA’s 2022, study titled Drugs and the Brain.
1. Dopamine
Dopamine is often associated with the brain’s reward system, playing a critical role in motivation, pleasure, and reinforcement learning.
Addictive drugs significantly increase dopamine levels in the brain’s reward pathways, leading to the reinforcement of drug use as a desirable behavior. Over time, the brain may reduce its own dopamine production or the number of dopamine receptors, diminishing the user’s ability to experience pleasure from natural rewards and leading to increased drug use to compensate.
Dopamine is often termed the “feel-good” neurotransmitter or the brains reward system. It’s released during pleasurable activities, reinforcing the desire to repeat them. Drug use elevates dopamine levels, thus hijacking the natural reward system. Over time, this leads to heightened cravings and dependency.
2. Glutamate
Glutamate is the main excitatory neurotransmitter in the brain, essential for cognitive functions like learning and memory.
Addiction disrupts glutamate homeostasis, which is crucial for the brain’s reward system and the ability to form memories associated with substance use. This disruption can contribute to craving and compulsive drug use behaviors.
3. GABA (Gamma-Aminobutyric Acid)
GABA serves as the primary inhibitory neurotransmitter in the brain, regulating excitability and playing a key role in relaxation and stress reduction.
Depressants, such as alcohol and benzodiazepines, enhance GABA activity, leading to decreased brain activity and a calming effect. Chronic use of these substances can alter GABAergic functioning, leading to tolerance and dependence.
4. Serotonin
Serotonin influences mood, emotion, sleep, and appetite and is linked to feelings of well-being and happiness.
Imbalanced serotonin levels can contribute to emotional instability, which often precedes addictive behaviors. Addictive substances directly impact serotonin levels, thereby affecting one’s emotional state and decision-making abilities.
Long-term drug use disrupts natural serotonin function, contributing to mood disorders and exacerbating addiction.
5. Norepinephrine
Norepinephrine acts as a neurotransmitter and hormone, playing a crucial role in the ‘fight or flight’ response, alertness, and concentration.
Stimulant drugs, such as cocaine and amphetamines, increase norepinephrine levels, leading to heightened alertness and energy. However, chronic use can disrupt normal norepinephrine function, affecting stress responses and arousal.
6. Endorphins
Endorphins are natural pain relievers and stress reducers, known as the body’s “natural opiates” due to their ability to induce feelings of pleasure and euphoria.
Endorphins act as natural painkillers and mood elevators. They’re released during exercise, stress, and pain. Some addictive substances mimic the effects of endorphins, creating a temporary sense of well-being but ultimately leading to a craving for the substance to sustain that feeling.
Opioid drugs mimic the effects of endorphins, binding to opioid receptors in the brain to reduce pain and produce euphoria. Over time, the brain may produce fewer endorphins, leading to dependence on opioids to achieve pain relief and pleasure.
7. Acetylcholine
Acetylcholine is involved in many functions, including muscle movement, heart rate, memory, and cognition.
Nicotine from tobacco products acts on acetylcholine receptors, leading to increased arousal, cognitive enhancement, and euphoria. Chronic nicotine use can lead to changes in acetylcholine receptor numbers and function, contributing to addiction and withdrawal symptoms.
8. Anandamide
Anandamide, often referred to as the “bliss molecule,” is a neurotransmitter that binds to cannabinoid receptors, influencing mood, memory, appetite, and pain.
THC, the psychoactive component of cannabis, mimics the effects of anandamide, leading to altered mood and perception. Chronic cannabis use can affect the endocannabinoid system’s natural function, leading to changes in mood, memory, and reward processing.
9. Oxytocin
Oxytocin is called the “love hormone,” because it plays a crucial role in social bonding, sexual reproduction, childbirth, and the period after childbirth. It’s also involved in behaviors like trust, empathy, and social recognition.
Oxytocin has been shown to influence social bonding and stress relief, and recent research suggests it may have a role in addiction by modulating the reward and stress systems in the brain. It affects the social context of drug use and could potentially be targeted for therapeutic interventions in addiction treatment.
10. Cortisol
Cortisol is known as the “stress hormone,” involved in the body’s stress response. It helps regulate metabolism, inflammation, and the sleep-wake cycle.
Elevated cortisol levels can result from chronic stress or substance use, leading to altered reward processing and increased susceptibility to addiction. High cortisol can also worsen withdrawal symptoms and contribute to relapse.
11. Dynorphins
Dynorphins are a class of opioid peptides that play a role in the body’s natural pain response and are also involved in mood regulation.
Dynorphins are released in response to stress and drug use and are thought to contribute to the dysphoria associated with drug withdrawal. They may regulate the balance of the reward system, influencing addiction’s reinforcing or aversive aspects.
12. Neuropeptide Y (NPY)
NPY is one of the most abundant neuropeptides in the brain, involved in regulating stress responses, anxiety, appetite, and energy balance.
NPY levels are affected by drug use and withdrawal. It has been suggested that NPY may have a protective role against the effects of stress on addiction and could be a potential target for treating addiction, particularly in reducing anxiety and stress-related relapse.
13. Vasopressin
Vasopressin, also known as antidiuretic hormone (ADH), plays a crucial role in regulating water balance in the body and has been implicated in social behavior, stress response, and pair bonding.
Similar to oxytocin, vasopressin influences social behaviors and stress responses related to addiction. Its role in addiction is less understood but is thought to interact with the brain’s reward and stress pathways, potentially influencing addiction dynamics and treatment outcomes.
14. Adrenaline
Adrenaline, also known as epinephrine, is a hormone and neurotransmitter produced mainly by the adrenal glands and certain neurons. It plays a pivotal role in the body’s fight-or-flight response to stressful or threatening situations, rapidly preparing the body for action. Adrenaline increases heart rate, elevates blood pressure, expands the air passages of the lungs, enlarges the pupil in the eye, and redistributes blood to the muscles, among other effects, essentially priming the body for physical exertion.
In the context of addiction, adrenaline’s role is multifaceted:
- Stress Response: Adrenaline is a key component of the stress response, which can influence substance use and addiction. Individuals may use drugs or alcohol as a way to manage or escape from the heightened physical and emotional states induced by adrenaline.
- Risk-Taking and Reward: The surge of adrenaline can enhance the sensation of risk-taking behaviors, which are often associated with the use of addictive substances. This can reinforce the behavior and contribute to the cycle of addiction, as individuals seek out experiences that stimulate the release of adrenaline and other reward-related neurotransmitters.
- Withdrawal and Craving: During withdrawal from addictive substances, changes in adrenaline levels can contribute to symptoms such as anxiety, agitation, and physical distress. These symptoms can drive the craving for the substance as a way to alleviate the discomfort, complicating the recovery process.
While adrenaline itself is not addictive, its effects on the body and its role in the stress response and reward system can interact with the pathways of addiction. Understanding the relationship between adrenaline and addiction can provide insights into the challenges of overcoming addictive behaviors and the importance of managing stress and emotional regulation as part of the recovery process.
| # | Neurotransmitter | Role in the Brain | Impact on Addiction |
|---|---|---|---|
| 1 | Dopamine | Associated with the brain’s reward system, critical for motivation, pleasure, and reinforcement learning. | Increases in dopamine levels due to addictive drugs reinforce drug use as a desirable behavior, leading to dependency and diminished ability to enjoy natural rewards. |
| 2 | Glutamate | Main excitatory neurotransmitter, essential for learning and memory. | Addiction disrupts glutamate homeostasis, affecting the brain’s reward system and contributing to craving and compulsive behaviors. |
| 3 | GABA (Gamma-Aminobutyric Acid) | Primary inhibitory neurotransmitter, regulating excitability and stress reduction. | Depressants enhance GABA activity, causing decreased brain activity and calmness, leading to tolerance and dependence. |
| 4 | Serotonin | Influences mood, emotion, sleep, and appetite, linked to well-being and happiness. | Imbalanced levels contribute to emotional instability and addictive behaviors, with long-term drug use exacerbating mood disorders. |
| 5 | Norepinephrine | Acts as a neurotransmitter and hormone, important for ‘fight or flight’ response, alertness, and concentration. | Stimulant drugs increase norepinephrine, leading to heightened alertness and energy but disrupting normal function over time. |
| 6 | Endorphins | Body’s natural pain relievers and stress reducers, inducing pleasure and euphoria. | Addictive substances mimic endorphins, leading to temporary well-being but eventual craving and dependence on opioids for pleasure. |
| 7 | Acetylcholine | Involved in muscle movement, heart rate, memory, and cognition. | Nicotine affects acetylcholine receptors, increasing arousal and cognitive enhancement, leading to addiction and withdrawal symptoms. |
| 8 | Anandamide | “Bliss molecule” that binds to cannabinoid receptors, affecting mood, memory, appetite, and pain. | THC mimics anandamide, altering mood and perception, with chronic use affecting the endocannabinoid system. |
| 9 | Oxytocin | “Love hormone” involved in social bonding, sexual reproduction, childbirth, and trust, empathy, and social recognition. | May influence addiction by modulating the reward and stress systems, affecting social contexts of drug use. |
| 10 | Cortisol | “Stress hormone,” regulating metabolism, inflammation, and the sleep-wake cycle. | Elevated levels from stress or substance use lead to altered reward processing and increased addiction susceptibility, worsening withdrawal and relapse. |
| 11 | Dynorphins | Opioid peptides involved in natural pain response and mood regulation. | Released in response to stress and drug use, contributing to withdrawal dysphoria and influencing the reward system. |
| 12 | Neuropeptide Y (NPY) | Regulates stress responses, anxiety, appetite, and energy balance. | Affected by drug use and withdrawal, with potential protective roles against stress effects on addiction. |
| 13 | Vasopressin | Regulates water balance and implicated in social behavior, stress response, and pair bonding. | Influences social behaviors and stress responses related to addiction, with potential impacts on addiction dynamics and treatment. |
| 14 | Adrenaline (Epinephrine) | Key hormone and neurotransmitter in the ‘fight or flight’ response, increasing heart rate, blood pressure, and energy supply. | Not typically discussed directly in the context of addiction, adrenaline surges can be associated with drug use, enhancing feelings of excitement and energy. However, it’s not primarily linked to the addiction cycle like dopamine or endorphins. |
For further reading and resources on addiction treatment, please refer to our Complete Guide to Addiction Treatment. Your journey to understanding and combating addiction starts here.
What Portions Of The Brain Are Affected By Drug Addiction?
Addiction impairs the prefrontal cortex’s decision-making and impulse control while making the amygdala more reactive to emotional states, fueling stress and anxiety, and finally the basal ganglia and its’s impact on motivation are key components in the cycle of dependency.
1. Prefrontal Cortex, Decision-Making:
This area of the brain controls executive functions, such as decision-making and impulse control. Addiction weakens the prefrontal cortex’s ability to resist urges, thereby compromising an individual’s capacity for self-control.
The compromised prefrontal cortex, weakened by addiction, struggles to perform its critical role in managing executive functions like decision-making and impulse control. This diminished capacity makes it challenging for individuals to resist the urges and cravings that are characteristic of addiction. As a result, the ability to make rational choices and exert self-control is significantly reduced, leading to a cycle where the immediate gratification provided by substance use overshadows long-term considerations and the negative consequences of such behaviors. This impairment in the prefrontal cortex not only fuels the continuation of substance abuse but also hinders the individual’s ability to engage effectively in treatment and recovery processes, making it a pivotal area of focus for overcoming addiction.
2. Amygdala, Emotional Response:
The amygdala governs our emotional responses and becomes hyperactive when addiction is present leading to heightened emotional states, particularly stress and anxiety, which often fuel the cycle of dependency.
The addicted person’s amygdala, being hyper-reactive due to substance use, exaggerates emotional responses, especially to stress and anxiety. This heightened state not only intensifies feelings of discomfort but also increases the likelihood of substance use as a misguided attempt to self-medicate and alleviate these negative emotions. Consequently, this creates a vicious cycle where the individual’s reliance on substances further sensitizes the amygdala, exacerbating emotional responses and reinforcing the dependency. This altered brain function makes recovery challenging, as it involves not only breaking the physical dependence on substances but also retraining the brain to manage emotional responses healthily.
3. Basal Ganglia, Movitation:
The basal ganglia, a critical structure within the brain, serve as the cornerstone for fostering positive forms of motivation. These include the pleasurable effects derived from engaging in healthy activities such as eating, socializing, and sexual interactions. Additionally, the basal ganglia are pivotal in the development and maintenance of habits and routines, positioning them as a central element of what is often referred to as the brain’s “reward circuit.”
When drugs are introduced into the system, they hyper-stimulate this reward circuit, leading to the euphoria commonly associated with the drug high. This over-activation not only highlights the immediate impact of substances on the brain but also underscores a significant alteration in the brain’s functioning over time. With repeated drug exposure, the reward circuit undergoes adaptation, reducing its sensitivity to stimuli. This process results in a diminished ability to experience pleasure from everyday activities, compelling individuals to seek out the drug to recapture the once-accessible feelings of euphoria.
Dysregulation of the brain emotional systems that mediate arousal and stress is a key component of the pathophysiology of drug addiction.
(Brain Res. 2009)
What Is The Role Of Nucleus Accumbens In The Brain Response To Addiction?
The Nucleus Accumbens plays a central role in the brain’s reward circuitry. Situated in the basal forebrain, this region acts as a key intersection for neurotransmitters like dopamine, which are essential for experiencing pleasure and reinforcing behaviors. In the context of addiction, substances or addictive behaviors stimulate the release of an unnaturally high amount of dopamine in the Nucleus Accumbens. This creates a sensation of intense pleasure or a “high,” which the brain then remembers and seeks to replicate.
Over time, the Nucleus Accumbens adapts to these elevated levels of dopamine, resetting the brain’s “pleasure baseline.” As a result, activities that once brought moderate joy no longer have the same impact, reinforcing the reliance on the addictive substance or behavior to reach this new, higher baseline of pleasure. This adaptation creates a cycle of dependency, where increasingly larger amounts of the substance or more frequent engagement in the behavior are required to achieve the same level of satisfaction.
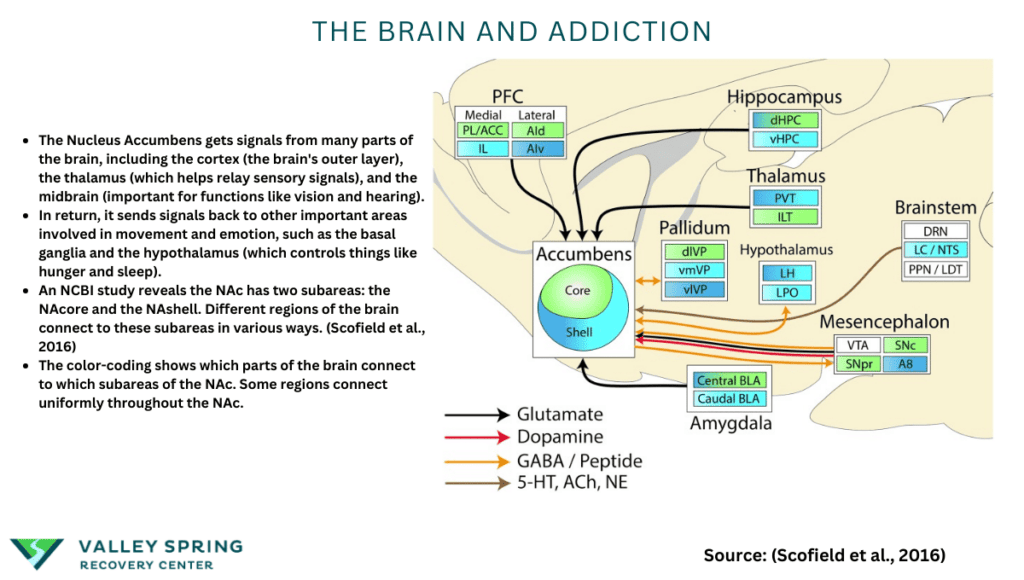
- The Nucleus Accumbens gets signals from many parts of the brain, including the cortex (the brain’s outer layer), the thalamus (which helps relay sensory signals), and the midbrain (important for functions like vision and hearing).
- In return, it sends signals back to other important areas involved in movement and emotion, such as the basal ganglia and the hypothalamus (which controls things like hunger and sleep).
- An NCBI study reveals the NAc has two subareas: the NAcore and the NAshell. Different regions of the brain connect to these subareas in various ways. (Scofield et al., 2016)
- The color-coding described in the article is a way to show which parts of the brain connect to which subareas of the NAc. Some regions connect uniformly throughout the NAc.
So, in essence, the NAc is like a busy traffic junction in the brain, receiving and sending signals to various places. These connections help it play its role in making us feel pleasure and rewarding certain behaviors.
Understanding the role of the Nucleus Accumbens in addiction helps to shed light on why individuals continue to seek out addictive substances or behaviors despite adverse consequences. This knowledge is crucial for developing targeted therapeutic approaches aimed at disrupting the maladaptive reward patterns facilitated by this brain region.
Addiction not only impacts specific neurotransmitters and brain regions but also fundamentally changes how the brain operates. This process is known as neuroplasticity, where the brain’s structure and function adapt over time. In the case of addiction, these adaptations are maladaptive, leading to long-term impairments in cognition, emotion, and behavior.
What Happens To The Brain During Withdrawal?
Withdrawal is a direct consequence of the brain adapting to a substance. When the substance is suddenly removed, it results in a myriad of symptoms ranging from anxiety and irritability to severe physical discomfort. This happens because the Central Nervous System has become reliant on the substance to maintain a perceived state of equilibrium.
Drug self-administration initially involves action-outcome learning fueled by the incentive value of the drug (goal-directed behavior) and is believed to then transition to habit formation elicited by stimuli that have taken on associative value. This is thought to underlie drug-seeking motivation according to Everitt and Robbins, 2005; and Hogarth et al., 2013.
Similar to Pavlovian conditioning, once someone becomes addicted to a substance and conditioned to take it, breaking the habit can be difficult and involves mental, physical, and behavioral transitions which can be painful.
What Is The Cycle Of Addiction?
The journey into and through addiction often follows a cycle: Initiation, Habituation, and Dependency.
- Initiation: The brain’s reward system is activated.
- Habituation: The reward system is repeatedly activated, causing neural adaptations.
- Dependency: The brain now requires the substance or behavior to function “normally.”
Understanding this cycle from a neurological standpoint is critical for both prevention and treatment.
FAQs about the Neuroscience of Addiction
What neurotransmitters are involved in addiction?
The main neurotransmitters implicated in addiction are Dopamine, responsible for the reward system; Serotonin, which regulates mood and emotion; and Endorphins, which act as natural painkillers and mood elevators. Understanding these neurotransmitters helps demystify why substances and behaviors become addictive.
How does addiction affect brain function?
Addiction fundamentally alters brain function by changing the way neurotransmitters communicate and affecting key regions like the Prefrontal Cortex, Amygdala, and Nucleus Accumbens. Over time, this results in maladaptive forms of neuroplasticity, leading to cognitive, emotional, and behavioral impairments.
Is addiction a disease or a choice?
From a scientific standpoint, addiction is considered a chronic disease. It involves alterations in brain structure and function, making it more than just a matter of choice or willpower. While initial exposure to a substance or behavior is often voluntary, the progression to addiction involves physiological changes that reduce an individual’s ability to control their actions.
Can brain damage from addiction be reversed?
Some neurological effects of addiction can be reversible through sustained abstinence and proper treatment, although the extent of reversibility depends on various factors like the substance involved, duration of addiction, and individual health conditions. Treatments like Medication-Assisted Treatment (MAT) and Cognitive Behavioral Therapy (CBT) are designed to mitigate and sometimes reverse these changes.
Why Does Drug Seeking Behavior Occur?
Chronic drug use disrupts the plasticity in the nucleus accumbens, which in turn allows drug-associated cues to create a pathological motivation for drug-seeking behavior.
What Is The Science of Addiction?
The Science Behind Addiction: Understanding the science of the brain and drug addiction is not just an academic exercise; it has profound implications for addiction treatment. The neurochemical imbalances, the role of the nucleus accumbens in reward and motivation, and the molecular basis for relapse all provide crucial insights into how addiction can be effectively treated. Treatment methodologies such as Medication-Assisted Treatment (MAT) can be more effective when tailored to target specific neurotransmitters or brain regions. Cognitive Behavioral Therapy (CBT) can be modified to address the weakened decision-making abilities caused by alterations in the prefrontal cortex.
Neuroplasticity and Treatment: The concept of neuroplasticity, the brain’s ability to adapt and change, is a double-edged sword in addiction. While it’s the mechanism that allows addiction to take hold, it’s also the basis for treatment strategies like Cognitive Behavioral Therapy (CBT) that aim to rewire the brain’s reward and coping mechanisms.
Targeting the Nucleus Accumbens: Pharmacological interventions often target the nucleus accumbens, the “pleasure center” of the brain, to modulate its activity. By understanding how this region responds to different classes of drugs, researchers can develop more effective medications that can either block the rewarding effects of drugs or substitute them with less harmful alternatives.
The Time Factor – Breaking Conditioning: Breaking the conditioning associated with drug addiction is a long-term process and varies from individual to individual. The time it takes to break this conditioning can range from weeks to years, depending on various factors like the duration of drug use, the type of drug, and the individual’s psychological makeup. This is why 90-day rehab centers are sometimes more successful than 30-day rehab programs and why patients who continue with outpatient treatment and therapy or peer recovery after they graduate have better outcomes. The molecular changes in the brain can persist long after drug use has ceased, making the individual susceptible to triggers and relapses. This is why long-term treatment plans that include both pharmacological and behavioral therapies are often the most effective.
The Neuroscience of Addiction In Broader Behavioral and Mental Health Contexts
In summarizing our exploration of the neuroscience of addiction, it becomes evident that this complex condition is deeply intertwined with various other behavioral and mental health disorders. The Nucleus Accumbens, a crucial player in addiction, also plays a significant role in other conditions like depression, anxiety, and Obsessive-Compulsive Disorder (OCD). The interconnectedness of brain structures like the Prefrontal Cortex, Amygdala, and Thalamus further broadens the spectrum of behaviors and emotions affected by addiction, cementing its status as a multifaceted neurological disorder rather than a simple act of willpower.
Addiction’s relationship with neurotransmitters such as dopamine and serotonin brings into focus its proximity to mood disorders and even certain personality disorders. This intrinsic link demands a holistic approach to treatment. Strategies such as Medication-Assisted Treatment (MAT) and Cognitive Behavioral Therapy (CBT) can be adapted to cater to this broader mental health spectrum, offering multi-pronged solutions that address the root causes rather than just the symptoms of addiction.
Furthermore, the maladaptive neuroplastic changes associated with addiction have comparable counterparts in disorders like PTSD, making this understanding pivotal not only for addiction treatment but for a comprehensive mental health strategy.
In the digital era, technology addiction demonstrates how this neural pathway of exploitation isn’t confined to substance abuse, extending our understanding of addiction into the realm of the modern age.
What Impact does serotonin have on addiction?
Serotonin, a key neurotransmitter involved in mood regulation, appetite, and sleep, has a significant impact on addiction in several ways:
- Mood Regulation: Serotonin’s role in mood regulation is critical. Low levels are associated with depression and anxiety, conditions often linked with substance use disorders. By influencing mood, serotonin can either exacerbate vulnerability to addiction or support recovery.
- Reward Pathways: While dopamine is directly linked to the brain’s reward system, serotonin also modulates this system. It can influence the rewarding effects of substances, affecting cravings and addiction behaviors.
- Impulse Control: Serotonin is involved in impulse control and decision-making. Dysregulation in serotonin levels can lead to impaired judgment and increased impulsivity, factors that contribute to the development and continuation of addictive behaviors.
- Stress Response: Serotonin helps regulate the body’s response to stress. High-stress levels can lead to increased substance use as a coping mechanism, while balanced serotonin levels can mitigate stress responses and reduce reliance on substances.
- Withdrawal and Relapse: Changes in serotonin levels during withdrawal can contribute to the severity of withdrawal symptoms. Effective management of these levels is crucial in minimizing discomfort and reducing the risk of relapse.
Understanding serotonin’s impact on addiction highlights the importance of comprehensive treatment approaches that address the complex interplay of neurotransmitters in recovery.
What Impact does Dopamine have on addiction?
Dopamine, often referred to as the “feel-good” neurotransmitter, plays a central role in addiction due to its impact on the brain’s reward system. Here’s how dopamine affects addiction:
- Reward and Pleasure: Dopamine is released in response to pleasurable activities, including eating, social interactions, and substance use. Drugs of abuse can cause a significant surge in dopamine, reinforcing the behavior and making the substance highly rewarding.
- Motivation and Compulsion: The dopamine surge from substance use increases motivation to repeat the experience. Over time, this can lead to compulsive substance seeking and use, a hallmark of addiction.
- Tolerance and Dependence: With repeated substance use, the brain adjusts to the excess dopamine by reducing dopamine receptor sensitivity or production. This leads to the need for more of the substance to achieve the same dopamine high, a process known as tolerance.
- Withdrawal Symptoms: Reduced dopamine levels during withdrawal can lead to feelings of sadness, emptiness, and decreased motivation, making withdrawal challenging and contributing to relapse.
- Brain Structure Changes: Chronic substance use can alter brain regions influenced by dopamine, affecting decision-making, self-control, and pleasure in everyday activities. These changes can perpetuate addiction and complicate recovery efforts.
Dopamine’s critical role in the reward system and its modulation by addictive substances underscores the complexity of addiction as a brain disorder, requiring comprehensive approaches for effective treatment and recovery.
What is Neuroplasticity and How Does It Relate to the Brain and Addiction?
Neuroplasticity, also known as brain plasticity, refers to the brain’s ability to change and adapt throughout an individual’s life. This capability encompasses the brain’s potential to reorganize itself by forming new neural connections in response to learning, experience, and environmental changes. Neuroplasticity is fundamental to the brain’s development from infancy through adulthood and plays a crucial role in learning new skills, recovering from brain injuries, and adapting to new situations.
Neuroplasticity is deeply intertwined with the process of addiction according to the NIDA study Drugs and the Brain. Substance use and addictive behaviors can significantly alter the brain’s structure and function, exploiting the brain’s plastic nature:
- Formation of Addictive Memories: Through neuroplastic changes, the brain associates substance use with pleasure or relief from discomfort, reinforcing drug-seeking behaviors. These changes strengthen neural pathways related to addiction, making cravings and relapse more likely.
- Alteration in Reward Circuitry: Addictive substances can hijack the brain’s reward system, leading to overstimulation of pathways involving neurotransmitters like dopamine. Neuroplastic changes may amplify the perceived value of the substance while diminishing the value of natural rewards.
- Adaptation and Tolerance: The brain’s adaptive response to repeated substance exposure can lead to tolerance, where higher doses of the substance are required to achieve the same effect. Neuroplasticity underlies these adjustments, as the brain attempts to maintain balance in its neurotransmitter systems.
- Impact on Cognitive Functions: Addiction can also affect cognitive functions such as decision-making, impulse control, and self-regulation, as neuroplastic changes occur in areas of the brain involved in these processes. Over time, these changes can contribute to the compulsive nature of addiction.
- Recovery and Rewiring: On a positive note, the principles of neuroplasticity also support the recovery process. Through therapeutic interventions, lifestyle changes, and supportive environments, individuals can rewire their brains, weakening the neural connections associated with addiction and strengthening those associated with healthier behaviors and coping mechanisms.
How does the habenula contribute to neuroplasticity in addiction, and what implications does this have for treatment strategies?
The habenula, a tiny brain structure located in the epithalamus, plays a critical role in the neuroplastic changes associated with addiction. Research suggests that the habenula is involved in processing negative experiences and the avoidance of adverse outcomes. It becomes particularly relevant in the context of addiction as it influences dopamine release, contributing to the brain’s reward and aversion systems.
In addiction, the habenula can affect the way an individual responds to the absence of a drug, potentially enhancing the negative emotions and stress associated with withdrawal. This response can exacerbate cravings and the risk of relapse. Understanding the habenula’s role in these processes highlights its potential as a target for therapeutic interventions. Treatments that could modulate the activity of the habenula might help mitigate these negative responses and support long-term recovery by altering the underlying neuroplastic changes induced by substance use.
The implications for treatment are significant, as targeting the habenula could lead to the development of new therapeutic strategies that specifically address the neuroplastic changes in the brain’s reward and aversion circuits. This could improve the effectiveness of existing treatments and provide new avenues for preventing relapse in individuals recovering from addiction.
Sources
- Scofield, M. D., et al. “The Nucleus Accumbens: Mechanisms of Addiction across Drug Classes Reflect the Importance of Glutamate Homeostasis.” Pharmacological Reviews, vol. 68, no. 3, July 2016, pp. 816-871, doi:10.1124/pr.116.012484.
- Everitt BJ, Robbins TW. Neural systems of reinforcement for drug addiction: from actions to habits to compulsion. Nat Neurosci. 2005 Nov;8(11):1481-9. doi: 10.1038/nn1579. Erratum in: Nat Neurosci. 2006 Jul;9(7):979. PMID: 16251991.
- Hogarth L, Balleine BW, Corbit LH, Killcross S. Associative learning mechanisms underpinning the transition from recreational drug use to addiction. Ann N Y Acad Sci. 2013 Apr;1282:12-24. doi: 10.1111/j.1749-6632.2012.06768.x. Epub 2012 Nov 5. PMID: 23126270.
- Koob GF. Brain stress systems in the amygdala and addiction. Brain Res. 2009 Oct 13;1293:61-75. doi: 10.1016/j.brainres.2009.03.038. Epub 2009 Mar 28. PMID: 19332030; PMCID: PMC2774745.
- NIDA. “Understanding Drug Use and Addiction DrugFacts.” National Institute on Drug Abuse, 6 Jun. 2018, https://nida.nih.gov/publications/drugfacts/understanding-drug-use-addiction Accessed 11 Sep. 2023.
Dr. Michael Olla
All author postsShare This Post