Reward Pathway of the Brain: Definition, Function, and Role in Addiction

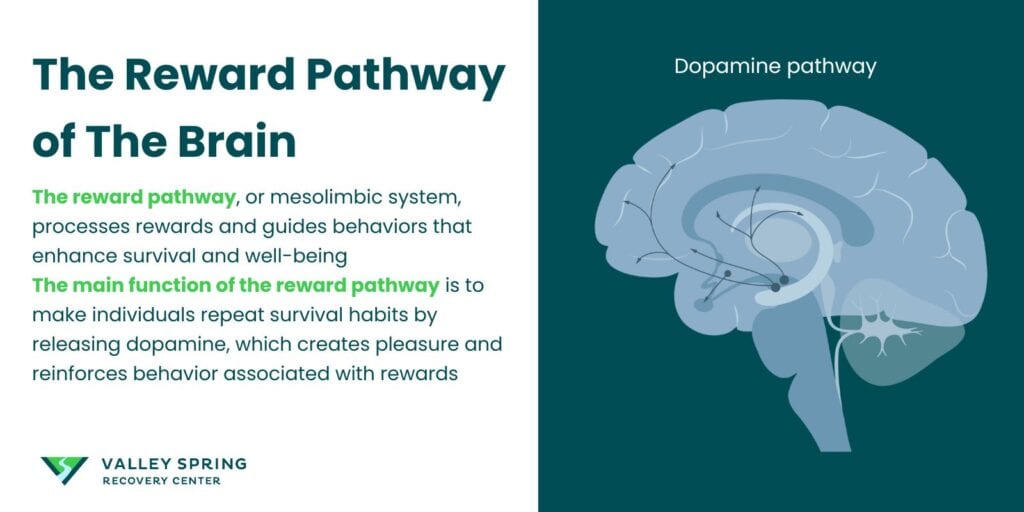
The brain’s reward pathway is a neural circuit primarily involving the mesolimbic dopamine system. It includes the ventral tegmental area, nucleus accumbens, and prefrontal cortex. According to a 2023 article by Olivia G-E, on the brain’s reward system published on Simply Psychology, the reward system structures are activated when a person experiences something pleasurable such as eating a nice meal. The system is responsible for regulating motivation, pleasure, and reinforcement learning.
The main function of the reward pathway is to tell individuals to repeat pleasure habits or actions to get rewards that are critical for survival such as food, or sex.
The reward pathway is vital for promoting adaptive behaviors, but it also becomes hijacked by drugs of abuse, leading to addiction. Addictive substances take over the brain’s reward system by causing a dopamine surge significantly greater than natural rewards, leading to a profound loss of control and changes in brain circuitry that make recovery challenging.
Recovery from addiction involves case management strategies that target the brain’s altered reward pathways, including medication-assisted treatment, behavioral therapies, lifestyle changes, and strong support systems. Cognitive-behavioral therapy and contingency management help addicts understand and modify thought processes leading to addictive behavior while reinforcing positive behavioral changes through rewards. Medications such as naltrexone, buprenorphine, and methadone modulate neurotransmission in the brain’s reward system, reducing cravings and withdrawal symptoms
What is The Reward Pathway of The Brain?
The reward pathway of the brain, also known as the mesolimbic system, is a sophisticated system of neural structures including the brain’s reward circuits. According to a 2021 study by Lewis, R. G., et al, on the brain’s reward system in health and disease, published in the Advances in Experimental Medicine and Biology journal, the reward pathway is responsible for the physical and cognitive processing of reward. The system guides people toward behaviors that enhance survival and well-being.
From the first bite of a savory meal to the joy of social interactions, this system rewards us with a surge of dopamine, reinforcing actions beneficial to our existence. However, in the shadow of substance addiction, this same reward system is subverted, transforming life-affirming activities into a destructive dependency on addictive substances. According to a 2011 study by Gardner EL, on addiction and brain reward and antireward pathways, addictive substances enhance the functioning of the reward circuitry of the brain. This produces a high that the substance user keeps seeking.
Did you know most health insurance plans cover substance use disorder treatment? Check your coverage online now.
What Is The Function Of The Reward Pathway?
The main function of the reward pathway is to tell individuals to repeat pleasure habits or actions to get rewards that are critical for survival such as food, or sex.
According to an article on the reward pathway published in the Genetic Science Learning Center journal, the primary function of the reward pathway is to make people repeat survival habits. When an individual engages in activities such as eating, drinking, or socializing, the brain releases dopamine, a neurotransmitter associated with pleasure and reward. This surge in dopamine activates the reward pathway, creating a sense of enjoyment and reinforcing the behavior that led to the pleasurable experience.
In addition, the reward pathway plays a crucial role in learning and memory. Dopamine release strengthens the connections between neurons, facilitating the formation of associations between stimuli and rewards. When you eat a nice meal, the reward pathways trigger the release of dopamine which gives you satisfaction. As a result of the nice feeling of satisfaction from the meal you got, you are likely to repeat the action in the future. This process, known as associative learning, enables individuals to anticipate and seek out rewarding experiences.
What is The Role of the Reward Pathway in Addiction?
The reward pathway is vital for promoting adaptive behaviors, but it also becomes hijacked by drugs of abuse, leading to addiction. Addictive substances, with their potent chemical properties, exaggerate the dopamine reward pathway, overwhelming the brain with a dopamine surge that is up to ten times greater than that triggered by natural rewards. This deluge of pleasure signals not only captivates the individual but also sets the stage for a profound loss of control over substance use, as the brain begins to prioritize the artificial high above all else.
One unique characteristic of addiction is the phenomenon of neuroadaptation, where repeated exposure to drugs induces changes in the brain’s reward circuitry. According to a 2022 article on how an addicted brain works, published in the Yale Medicine newsletter, prolonged drug use changes the sensitivity of dopamine receptors and reduces the brain’s ability to produce dopamine naturally. As a result, individuals experience diminished pleasure from everyday activities and require increasingly larger doses of the drug to experience the same euphoric effects.
In addition, drugs of abuse often stimulate the release of dopamine within the reward pathway directly, bypassing the need for natural rewards. This artificial activation of the reward system creates a powerful incentive for continued drug use, as individuals seek to replicate the intense pleasure associated with drug consumption.
The role of the reward pathway in addiction extends beyond mere pleasure-seeking behavior. According to a 2006 study by Verdejo-García, A., et al, on emotion, decision-making, and substance dependence, substance-dependent people exhibit signs of impairment in their decision-making. Chronic drug use leads to profound changes in decision-making, impulse control, and emotional regulation, impairing the individual’s ability to resist cravings and make rational choices. Additionally, alterations in the prefrontal cortex, a key component of the reward pathway, contribute to deficits in executive function and inhibitory control observed in individuals with substance use disorders.
Which Brain Regions Are Impacted by Addiction?
Addiction’s stealthy nature is revealed through its comprehensive impact on multiple areas of the brain. The ventral tegmental area (VTA) and the nucleus accumbens stand at the heart of the brain’s reward circuitry, orchestrating the release of dopamine in response to addictive substances. Meanwhile, the prefrontal cortex (PFC) projects its influence across these and other brain areas, grappling with aspects of memory, emotion, and stress associated with addiction.
The nucleus accumbens, receiving projections from the lateral hypothalamus, work in tandem with dopamine to regulate responses to psychostimulants, while the activation of orexin receptor 1 within this region is linked to the rewarding effects of such stimulation. The hippocampus, though not a primary reward structure, plays a critical role in forming memories that associate drug cues with their effects, particularly relevant during the anticipation stage of addiction.
As these regions become mired in the addiction process, the individual often experiences a profound loss of control over their urges, a testament to the powerful grip that addiction can have on the brain’s intricate reward system.
Contact us today to schedule an initial assessment or to learn more about our services. Whether you are seeking intensive outpatient care or simply need guidance on your drug addiction journey, we are here to help.
How is The Mesolimbic Dopamine Pathway Involved in Addiction?
The mesolimbic dopamine pathway, frequently regarded as the most crucial reward pathway in the brain, plays a key role in the story of addiction, [Adinoff, B.,2004]. This conduit, connecting the ventral tegmental area with the nucleus accumbens, facilitates the flow of dopamine that informs our brain’s reward system, influencing goal-oriented behaviors and the pursuit of pleasure. Additionally, the mesocortical dopamine pathway is another significant component of the brain’s mesolimbic dopamine system, which encompasses the reward system as a whole.
The chronic and potentially permanent changes that occur within this pathway due to the overwhelming release of dopamine by drugs underscore its central role in addiction. As we break down the components of this pathway, we will gain a deeper understanding of its influence in perpetuating addictive behavior.
Ventral Tegmental Area (VTA)
The ventral tegmental area (VTA) acts as the foundation for dopamine production in response to rewarding stimuli. Primarily composed of dopaminergic neurons, the VTA is instrumental in regulating:
- Reward
- Learning
- Memory
- Behaviors associated with addiction
The complex interplay of GABA cells and endocannabinoid signaling within the VTA exemplifies the nuanced mechanisms that govern dopamine release.
These dopaminergic and glutamatergic projections extend to areas such as the nucleus accumbens, reinforcing reward and influencing behaviors from wakefulness to defensive responses. Understanding the VTA’s role offers critical insights into the biological underpinnings of addiction and the challenge of mitigating its influence.
Nucleus Accumbens (NAc)
The nucleus accumbens (NAc) functions as a central hub in the brain’s reward processing system. The NAc has several important functions:
- It integrates limbic and cortical information
- It orchestrates goal-oriented behaviors
- It regulates actions related to reward through its connection to basal ganglia nuclei
The arrival of dopamine signals reward anticipation and primes the brain for new experiences, while glutamate plays a vital role in reinforcement learning, with its levels intricately affecting this process.
The nucleus accumbens, thus, acts as a key detector, parsing environmental stimuli and determining their reward value, ultimately driving the pursuit of pleasurable sensations and reinforcing substance-seeking behavior.
Rediscover Life at Valley Spring Recovery Center
Get the compassionate support you deserve. We're here to help you reclaim joy, wellness, and a brighter future.
Verify Benefits
Prefrontal Cortex (PFC)
The prefrontal cortex (PFC), a part of the cerebral cortex, operates as the brain’s command center, supervising decision-making processes that are vital in the context of addiction. It aids in linking pleasurable outcomes with the stimuli and actions that produced them, a function key to the development of addictive behaviors. Within the PFC lies a delicate balance between the ‘Go system’, which drives habitual substance seeking, and the ‘Stop system’, which inhibits such behaviors, with imbalances contributing to the persistence of addiction.
Despite the neurobiological changes wrought by addiction, the pre-frontal cortex enables some individuals to make conscious decisions to resist addictive behaviors, highlighting its potential role in recovery. The glutamatergic projections sent from the VTA to the PFC trigger excitatory responses in PFC neurons, critical for evaluating prediction errors and adjusting behavior accordingly.
How Does Addiction Progress From Initial Use to Compulsive Behavior?
Addiction progresses through a series of linked stages, each amplifying the next and deepening the impact of the addiction. This progression from initial use to compulsive behavior is a harrowing journey marked by the brain’s relentless pursuit of the substance, despite the negative effects on the individual’s life.
The efficiency of the prefrontal cortex declines during addiction, leading to compromised decision-making and heightened impulsivity. With each stage, the addiction strengthens its hold, tightening the grip on the individual’s ability to resist the lure of the substance.
Initial Drug Use
The path into addiction usually starts with the first use of a substance, triggering the brain’s reward system to generate pleasurable effects. The massive dopamine release, far exceeding that of natural rewards, lays the foundation for powerful urges to continue substance use, known as incentive salience.
This first encounter with a drug can lead to behaviors becoming firmly entrenched in the brain, influencing decision-making, learning, and memory processes beyond the reward system’s domain. It is this initial brush with an addictive substance that can set the stage for a long-term struggle with addiction.
Are you covered for treatment?
Valley Spring Recovery Center is an approved provider for Blue Cross Blue Shield and Cigna, while also accepting many other major insurance carriers.
Check Coverage Now!Repeated Exposure
With prolonged use, addictive substances cause the brain’s circuits to adjust, reducing their sensitivity to dopamine and requiring increased doses to attain the same level of pleasure. These neuroadaptations foster the shift from controlled use to chronic misuse and potential addiction.
As the individual continues to indulge in the substance, changes in receptors on dopamine neurons contribute to tolerance and the compulsion to increase drug intake for the same effects. The dorsal striatum, a brain structure integral to habit formation, plays a significant role in developing compulsive substance-seeking behavior as addiction escalates. Additionally, the ventral striatum is involved in the reward system, which can be affected by substance abuse.
The reward system’s diminished response to both addictive substances and natural rewards fuels a compulsive escalation in substance use, pushing the individual further into the depths of addiction.
Compulsive Drug Use and Relapse
Compulsive substance use and the likelihood of relapse are characterized by irreversible alterations in brain structure and diminished cognitive abilities. The memory of the intense dopamine surge from addictive substances can drive compulsive cravings over time, marking the transition from impulsive to compulsive drug-seeking behaviors.
Repeated drug use is linked with reduced levels of D2 receptors in the striatum, correlating with impaired function in the prefrontal regions critical for self-control, [Volkow ND,2001].This impairment in cognitive functions such as focus, memory, learning, decision-making, and judgment is crucial for exercising self-control and making healthy choices.
The damage to the prefrontal cortex (PFC) wrought by addiction leads to difficulty in controlling impulsive and compulsive behaviors, significantly contributing to the challenge of overcoming addiction. Additionally, the amygdala and associated networks play a role in the emotional and stress response during withdrawal, triggering cravings and relapse.
What Are The Recovery Strategies For Healing The Altered Reward Pathways?
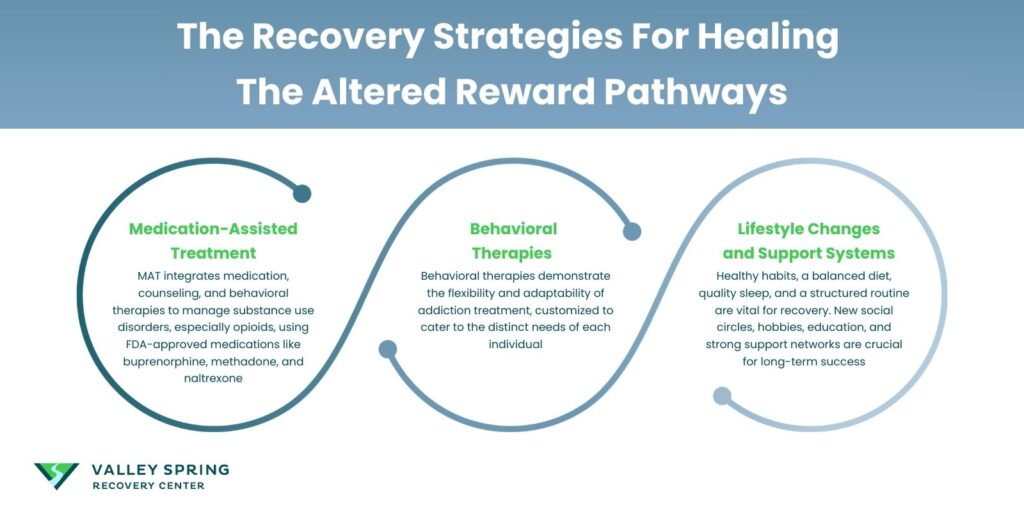
The recovery strategies of healing the altered reward pathways are medication-assisted treatment (MAT), cognitive-behavioral therapy, and contingency management. Cognitive-behavioral therapy and contingency management help addicts understand and modify thought processes leading to addictive behavior while reinforcing positive behavioral changes through rewards. Medications such as naltrexone, buprenorphine, and methadone modulate neurotransmission in the brain’s reward system, reducing cravings and withdrawal symptoms.
Did you know most health insurance plans cover substance use disorder treatment? Check your coverage online now.
1. Medication-Assisted Treatment
Medication-assisted treatment (MAT) forms an integral part of recovery, integrating medication, counseling, and behavioral therapies to effectively manage substance use disorders, especially opioid use disorders (OUD). MAT employs FDA-approved medications such as buprenorphine, methadone, and naltrexone, which have been demonstrated to be safe and effective when used alongside psychosocial support.
According to a 2017 article by Jennifer C., on new ways to help people beat opioid addiction, published in the Yale Medicine newsletter, clinicians and researchers at Yale School of Medicine advocate a medicine-assisted approach to dealing with opioid addiction. David A. Fiellin, MD, one of the principal authors of the study and specialist in addiction medicine at Yale School of Medicine says “Research shows that medication-based treatments are the most effective treatment. Opioid use disorder is a medical condition just like depression, diabetes or hypertension, and as with those conditions, it is most effectively treated with a combination of medication and counseling.”
Buprenorphine, a key player in the treatment of opioid dependence, can be administered in various forms, including sublingual tablets and extended-release injections, providing flexibility in meeting individual needs. Methadone and naltrexone also play pivotal roles, with methadone used orally and naltrexone available as an extended-release injectable, underlining the diverse treatment options available to combat addiction.
The FDA’s encouragement of the development of novel and more effective MAT options reflects a broader understanding of OUD as a chronic disease and a commitment to breaking the stigma often associated with these life-saving medications.
2. Behavioral Therapies
Behavioral therapies demonstrate the flexibility and adaptability of addiction treatment, customized to cater to the distinct needs of each individual.
- Cognitive-behavioral therapy (CBT): It plays a pivotal role by helping patients understand and change the behaviors and thought patterns related to drug use, offering a path to lasting change. According to a 2010 study by McHugh, R. K., et al, on cognitive-behavioral therapy for substance use disorders, published in the Psychiatric Clinics of North America journal, CBT as a standalone therapy or in combination with others, is highly effective in treating substance abuse disorders.
- Contingency Management (CM): According to a 2011 study by Petry, N. M., on Contingency management: what it is and why psychiatrists should want to use it, published in The Psychiatrist Journal, contingency management is ideal for treating substance use and other related disorders. This is a behavioral therapy where addicts are rewarded when there is evidence of abstinence. CM is based on a simple principle: reinforced behavior will increase in frequency. During substance abuse rehabilitation, CM interventions usually involve issuing monetary-related rewards whenever the recovering addict successfully submits drug-negative specimens.
3. Lifestyle Changes and Support Systems
Embracing healthy lifestyle habits is an essential aspect of recovery, complementing treatment approaches. A well-balanced diet, quality sleep, and a structured routine lay the foundation for both physical and emotional healing in individuals overcoming addiction.
Forming new social circles, engaging in hobbies, focusing on education and employment, and reflecting on spiritual and personal values are instrumental in forging a fulfilling, substance-free life. The significance of a strong support network—including peers, family, and structured environments like sober living homes—cannot be overstated, as they provide emotional support and play a vital role in relapse prevention, greatly contributing to successful long-term recovery.
Contact us today to schedule an initial assessment or to learn more about our services. Whether you are seeking intensive outpatient care or simply need guidance on your drug addiction journey, we are here to help.
How Can We Prevent Addiction by Targeting the Reward Pathway?
Prevention strategies focus on reducing exposure to drugs, especially during adolescence when the brain is still developing and more vulnerable to addiction. Education about the risks of drug use, fostering supportive environments, and promoting healthy activities that naturally engage the reward pathway help mitigate the risk of addiction. Research continues to explore how genetic and environmental factors interact to influence the reward pathway and susceptibility to addiction. According to a 2020 study by Volkow N.D., addiction is a complex brain disease, Nora holds that drugs such as marijuana change the endogenous cannabinoid system. Since most people experiment with drugs in their teenage, the results changing a developing brain’s endogenous cannabinoid system contributes to future vulnerability to substance abuse.
Is Addiction a Sign of Weakness or Failure?
No. Addiction is not a sign of weakness or failure. Rather addiction is a disease like asthma or hypertension. However, some people are more vulnerable to substance abuse disorders compared to others due to their genes, or environment. According to Nora D. Volkow, M.D., Director of the National Institute on Drug Abuse (NIDA), “There are people [whose genetic susceptibility is] so powerful [that it] overpower resilient environments, making them liable to addiction, and there are environments that are so stressful and adverse that [they] make people vulnerable to become addicted, even though they don’t have the genetic [susceptibility].”
Can Addiction Be Treated Successfully?
Yes, addiction is treated successfully using medication, psychotherapy, and social support. However, according to an article from the National Institute on Drug Abuse (NIDA) on understanding drug use and addiction drug, there is a possibility for people who have gone through treatment successfully to relapse.
Rediscover Life at Valley Spring Recovery Center
Get the compassionate support you deserve. We're here to help you reclaim joy, wellness, and a brighter future.
Verify Benefits
How does the reward pathway in the brain differ in individuals with addiction compared to those with a normal brain?
The reward pathway in the brain differs in individuals with normal and addicted brain. In individuals with addiction, the reward pathway in the brain becomes altered and hypersensitive to the presence of addictive substances. Normally, the reward pathway, involving key areas such as the nucleus accumbens, ventral tegmental area (VTA), and prefrontal cortex, functions to reinforce behaviors essential for survival by releasing dopamine, a neurotransmitter associated with pleasure and reward. However, in those with addiction, repeated substance use floods the brain with dopamine, leading to adaptations such as reduced dopamine receptor availability and altered neurotransmitter levels. This results in diminished pleasure from natural rewards and increased cravings for the addictive substance.
What are the key neurotransmitters involved in the reward pathway, and how do they contribute to addiction?
The reward pathway involves several key neurotransmitters in the brain affected by addiction. Dopamine is the primary neurotransmitter, driving the pleasure and reinforcement experienced from addictive substances. Serotonin, which influences mood and emotion, also interacts with the reward system and can be affected by substance use, contributing to mood swings and depression associated with addiction. Glutamate, involved in learning and memory, can reinforce the association between substance use and environmental cues, making it harder to break the cycle of addiction.
How can understanding the brain’s reward pathway inform the development of new addiction treatments?
Understanding the brain’s reward pathway can significantly inform the development of new addiction treatments by identifying specific targets for intervention. By mapping how addictive substances alter the function and structure of the reward pathway, researchers can develop pharmacological treatments that restore normal neurotransmitter levels and receptor activity. For example, medications that modulate dopamine levels or block the effects of addictive substances on the reward pathway can reduce cravings and withdrawal symptoms. Additionally, this knowledge can enhance behavioral therapies by identifying which cognitive strategies are most effective in rewiring the brain’s response to rewards. Combining pharmacological and behavioral approaches based on an in-depth understanding of the reward pathway can lead to more effective and personalized addiction treatments.
Are you covered for treatment?
Valley Spring Recovery Center is an approved provider for Blue Cross Blue Shield and Cigna, while also accepting many other major insurance carriers.
Check Coverage Now!How Can I Know If I’m At Risk Of Addiction?
You can know if you are vulnerable to substance abuse disorder if someone in your family is addicted or has substance abuse disorder. In addition, According to an article from the Mayo Clinic, on drug addiction (substance use disorder), peer pressure, and the existence of mental disorders increase the risk of drug addiction as well as genetic and hereditary predispositions increase addiction potential.
What Are The Signs Of Drug Addiction?
Signs of drug addiction include bloodshot eyes, dilated pupils, euphoria, and problems at work or school. According to a 2021 article from the National Institute on Drug Abuse (NIDA, other symptoms of substance abuse disorder include socializing with uncommon friends, losing interest in hobbies and social events, a change in sleeping or eating patterns, and neglect of personal hygiene.
What is an example of a brain reward pathway?
The mesolimbic dopamine system, composed of the VTA and NAc, is an important brain reward pathway that detects rewarding stimuli.
Did you know most health insurance plans cover substance use disorder treatment? Check your coverage online now.
What dopamine pathways are relevant in drug addiction?
The mesolimbic dopamine pathway, involving the ventral tegmental area (VTA) and nucleus accumbens, is relevant in drug addiction. This pathway is central to the addictive effects of substances and facilitates the process of addiction.
What are the pathways of addiction in the brain?
The pathways of addiction in the brain include the mesolimbic dopamine pathway and the striatum-thalamic-orbitofrontal circuit, which are involved in the compulsive drive for substances. These pathways play a significant role in the development of addiction.
How do addictive substances affect the brain’s reward system?
Addictive substances hijack the brain’s reward system by introducing unnatural levels of dopamine, leading to a loss of control over urges to abuse substances and causing neuroplastic changes in brain reward regions. This can result in compulsive substance abuse and addiction.
Contact us today to schedule an initial assessment or to learn more about our services. Whether you are seeking intensive outpatient care or simply need guidance on your drug addiction journey, we are here to help.
What is the importance of lifestyle changes in addiction recovery?
Lifestyle changes are crucial in addiction recovery as they reinforce healthy habits, build supportive networks, and create an environment for long-term recovery. These changes complement clinical treatments and support a successful recovery.
Share This Post















