Recent data from the Substance Abuse and Mental Health Services Administration (SAMHSA) reveal that as of 2023, approximately 19.7% of adults in the United States have encountered a substance use disorder. This prevalent condition manifests through a compelling urge to use drugs despite harmful consequences, and is influenced by genetic, environmental, and psychological factors. It’s a complex condition, not limited by social or economic backgrounds.
Drug addiction leads to physical and mental health issues like liver damage and increased depression risk, along with social and economic repercussions. Treatment is multifaceted, involving detox, rehab, and therapy, emphasizing the necessity of supportive care for effective recovery.

This article has been enhanced with input from the Medical Director and Addiction Psychiatrist at Valley Spring Recovery Center, Dr. Michael Olla.
Check the end of each section for extra information from him.
What Is Drug Addiction?
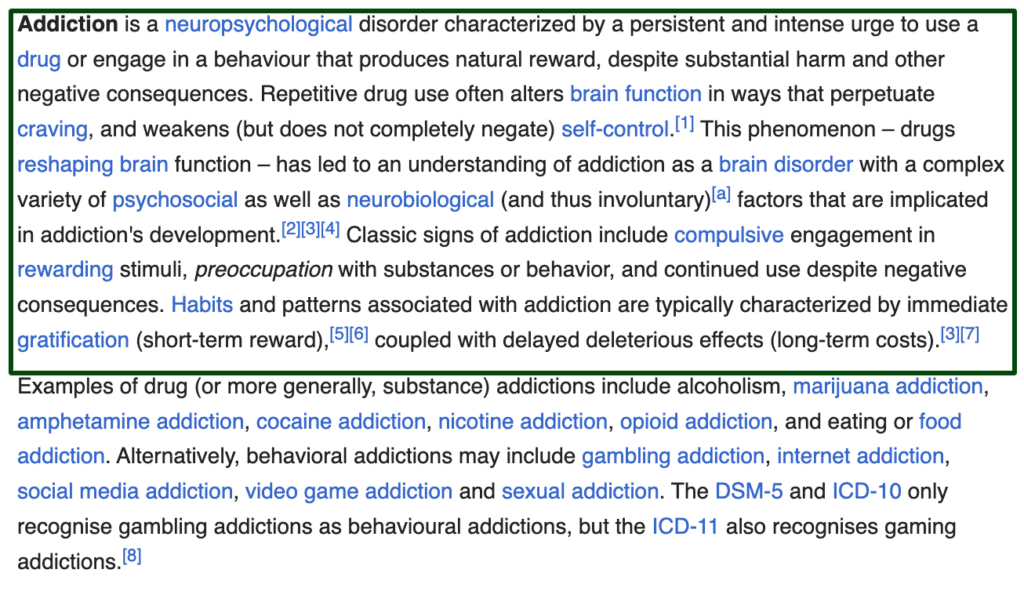
Drug addiction, clinically recognized as substance use disorder, is a chronic, relapsing brain condition that compels an individual to seek and use drugs despite adverse consequences. It is defined by alterations in the brain’s structure and function, leading to compulsive behaviors, impaired judgment, and prioritization of drug use.
Research from March 2022 by the National Institute on Drug Abuse (NIDA) titled “Drugs and the Brain” illustrates that addiction manipulates the brain’s reward system by significantly increasing levels of dopamine—a neurotransmitter linked to pleasure and reward. This surge in dopamine reinforces the drug use behavior, creating a cycle of addiction that can be challenging to break. This process results in what is often referred to as a ‘high,’ pushing individuals to continually seek out that intense feeling despite potential repercussions.
Addiction is further characterized as a brain disorder due to the lasting changes it induces in various neural circuits, particularly those related to reward, stress, and self-control. According to Goldstein RZ and Volkow ND’s 2011 study published in “Nature Reviews Neuroscience,” these changes can persist well beyond the cessation of drug use, significantly affecting an individual’s ability to make decisions and regulate behavior. This highlights the profound impact of addiction that extends beyond physical symptoms to include enduring brain alterations.
The prevalence of substance use disorder is startlingly high, impacting a significant portion of the population. According to the 2022 United States National Survey on Drug Use and Health (NSDUH), approximately 46.8 million Americans aged 12 and older, which accounts for 16.7% of this age group, battled a substance use disorder in the past year. This statistic underscores the critical need for comprehensive strategies to prevent and treat substance use disorders across the nation.
What is the difference between behavioral addictions and drug addictions?
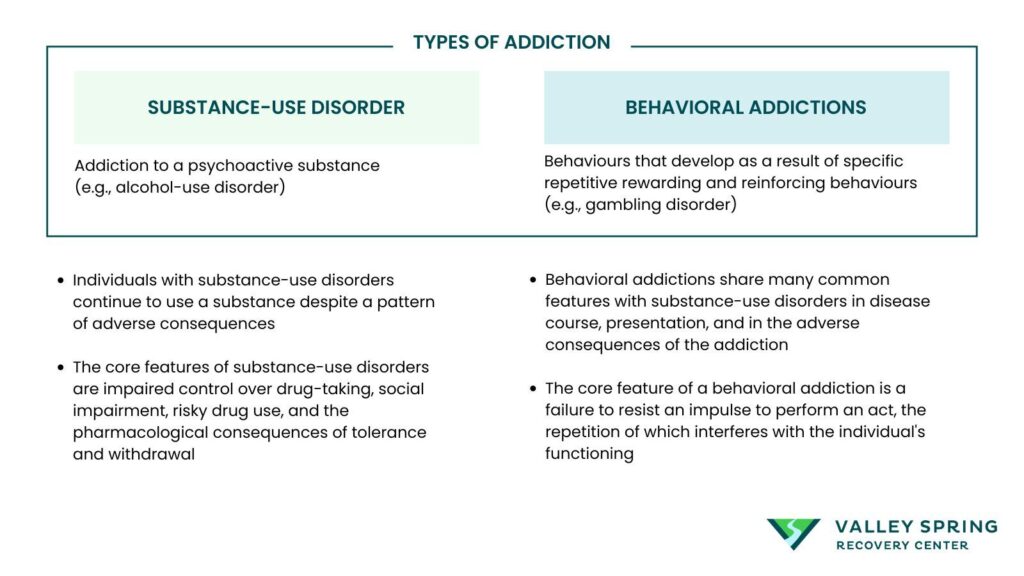
Behavioral addictions are different from drug addictions because they center around compulsive engagement in activities that do not involve substance consumption but still activate the brain’s reward systems similarly to psychoactive substances. According to Alavi, Seyyed Salman et al. (2012), behavioral addictions—such as gambling, overeating, television compulsion, and internet addiction—mirror drug addiction in that individuals are not addicted to a substance per se but to the behavior and the feelings derived from these activities. These compulsions induce pleasure or relieve negative emotions, much like the euphoria or escape provided by drugs, despite not involving tangible substances that alter brain chemistry.
Drug addictions, on the other hand, involve the actual intake of psychoactive substances like alcohol, nicotine, or illegal drugs. These substances chemically modify brain function and structure, directly impacting the brain’s reward system by elevating dopamine levels, leading to the reinforcement of drug use behaviors and significant changes in the brain’s neural circuits related to reward, stress, and self-control.
While drug addictions are linked to physical health effects and often require specific medical treatments including detoxification, behavioral addictions also necessitate comprehensive treatment approaches. Despite their lack of a chemical trigger, behavioral addictions can create similar patterns of dependency and withdrawal, demanding interventions focused on psychological support and lifestyle modifications. Both types of addictions require equally rigorous and structured treatment strategies, underlining the powerful impact of both substance-related and non-substance-related compulsive behaviors on mental health and daily functioning.
Is Addiction a Disease or a Choice?
Addiction is a chronic relapsing disease of the brain. The subject is widely debated with many dissenting opinions, but according to doctors and medical research, drug addiction is a disease and not a choice. Drug addiction It’s characterized by compulsive substance use despite harmful consequences. While the initial decision to use a substance may be voluntary, repeated use can lead to changes in the brain that impair self-control and hamper the ability to resist cravings, making it a medical condition rather than a mere choice.
Not all behavioral addictions are classified as a disease though. The Diagnostic and Statistical Manual of Mental Disorders (DSM) recognized behavioral addictions for the first time in DSM-5 with gambling disorder, formerly pathological gambling, as the only non-substance-related disorder classified under the chapter of “Substance-Related and Addictive Disorders”.
What’s the Difference Between Dependence and Addiction?
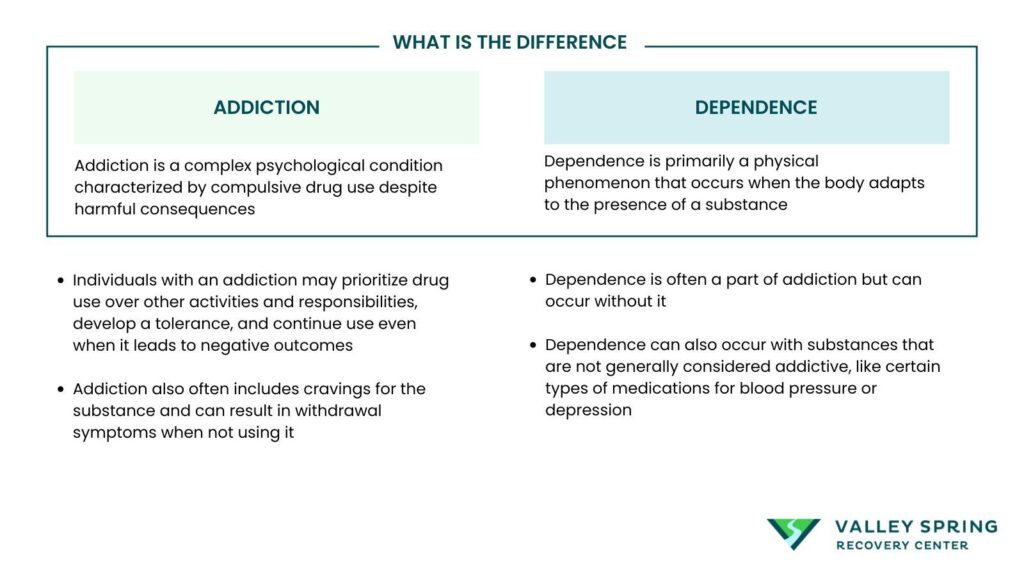
Dependence refers to the physical reliance on a substance, often marked by withdrawal symptoms when the substance is not taken. Addiction, on the other hand, is a broader concept that includes not only physical dependence but also psychological factors like cravings, loss of control, and continued use despite negative consequences.
Can You Be Addicted to Behaviors, Not Just Substances?
Addiction is not limited to substance abuse and includes behavioral addictions, such as gambling, shopping, or internet addiction, can also have detrimental effects on one’s life. These addictions trigger the reward system in the brain like substance abuse, leading to compulsive behaviors.
What Is The Criteria For Drug Addiction?
The criteria for addiction are characterized not merely by physical dependence but also by behavioral and psychological factors. The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), provides a standardized framework used by healthcare professionals to diagnose substance use disorders.
The criteria that constitute a substance use disorder according to the DSM-5 are listed below.
- Substance Use in Larger Amounts or Over a Longer Period: Individuals often take the substance in larger amounts or over a longer period than was originally intended.
- Persistent Desire or Unsuccessful Efforts to Cut Down: There is a persistent desire or unsuccessful attempts to cut down or control substance use.
- A Great Deal of Time Spent in Activities Necessary to Obtain, Use, or Recover: A considerable amount of time is spent in activities necessary to obtain the drug, use the drug, or recover from its effects.
- Craving, or a Strong Desire or Urge to Use the Substance: Individuals experience a strong desire or urge to use the substance, which often overtakes their ability to focus on normal daily activities.
- Recurrent Substance Use Resulting in a Failure to Fulfill Major Role Obligations: This includes failure to meet responsibilities at work, school, or home.
- Continued Use Despite Having Persistent or Recurrent Social or Interpersonal Problems: The individual continues to use substances despite having ongoing social or interpersonal problems exacerbated by the effects of the drug.
- Important Social, Occupational, or Recreational Activities Given Up or Reduced: Key social, occupational, or recreational activities are given up or reduced because of substance use.
- Recurrent Substance Use in Situations in Which It Is Physically Hazardous: This includes using substances under conditions where it is physically dangerous to do so, such as driving while under the influence.
- Use Continues Despite Knowledge of Having a Persistent or Recurrent Physical or Psychological Problem: The individual continues to use the substance despite awareness of having ongoing physical or psychological problems likely caused or exacerbated by the substance.
- Tolerance: This is defined by either a need for markedly increased amounts of the substance to achieve intoxication or desired effect, or a markedly diminished effect with continued use of the same amount of the substance.
- Withdrawal: The substance is taken to relieve or avoid withdrawal symptoms, and there are physiological withdrawal symptoms when the substance is not taken.
These criteria are not to be taken individually but rather considered collectively to diagnose substance use disorders. The presence of at least two of these symptoms within a 12-month period may indicate a substance use disorder. Severity is gauged by the number of criteria met: mild (2-3 criteria), moderate (4-5 criteria), and severe (6 or more criteria). Understanding these criteria helps in recognizing the depth and extent of an addiction, guiding toward appropriate treatment and support strategies.
What Are The Stages Of Addiction?
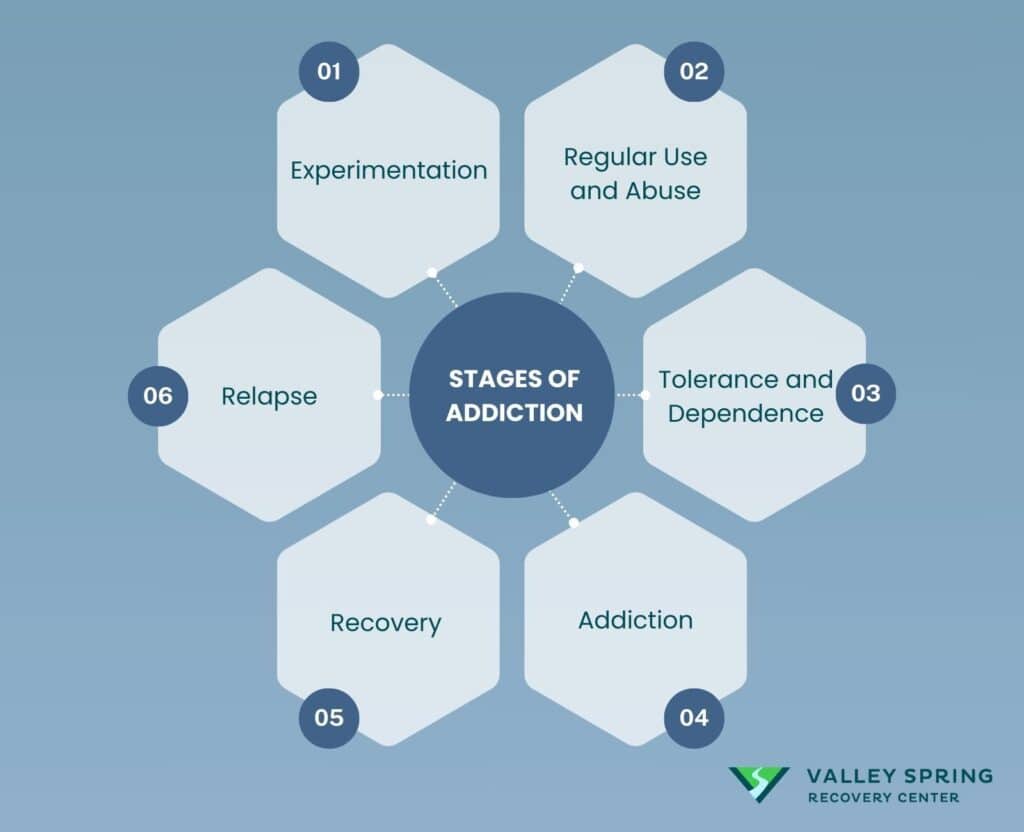
Addiction progresses through stages from initial experimentation due to curiosity or peer pressure, to regular use and abuse, developing tolerance and dependence, reaching compulsive addiction, moving through recovery efforts, and sometimes experiencing relapse, with each stage requiring tailored intervention strategies.
- Experimentation: Experimentation is typically the first stage of addiction, where individuals use substances occasionally out of curiosity, peer pressure, or to seek pleasure. During this phase, use is infrequent and, in some cases, may not progress any further. The National Institute on Drug Abuse (NIDA, 2020) notes that genetic factors can significantly affect whether an individual moves beyond this stage.
- Regular Use and Abuse: As use becomes more frequent, the transition from experimentation to regular use and then to abuse can occur. This stage is characterized by the increasing priority given to substance use over other activities, despite the awareness of adverse consequences. For some, substance use becomes a key method for coping with problems or emotions, escalating the risk of progressing to more severe stages.
- Tolerance and Dependence: Continuous and increased substance use leads to tolerance, where the body requires higher doses of the substance to achieve the initial effects. Dependence can be psychological or physical, indicating that the body has adapted to the substance’s presence. Withdrawal symptoms will appear if substance use is reduced or stopped, signaling physical dependence.
- Addiction: Addiction is marked by the inability to stop using the substance despite harmful physical, psychological, and social consequences. At this stage, the use is compulsive and out of control. Addiction impacts various aspects of an individual’s life, including relationships, work, and health.
- Recovery: Recovery involves actively engaging in treatment and recovery activities to overcome addiction. This can include therapy, medication-assisted treatment, and support groups. Recovery is an ongoing process and often requires lifelong commitment and support to maintain sobriety.
- Relapse: Relapse is not uncommon and should be considered a part of the process rather than a failure. It occurs when an individual returns to substance use after a period of abstinence and often highlights the need for continued or adjusted treatment strategies.
Understanding the stages of addiction is crucial for recognizing the signs of addiction and intervening effectively. Each stage may require different treatment approaches, emphasizing the need for personalized care tailored to the individual’s specific situation. According to NIDA (2020), effective treatment must address all aspects of addiction, not just substance use, to improve recovery outcomes and reduce the likelihood of relapse.
What Are The Types of Drug Addiction?
Drug addiction, often referred to as substance use disorder, can involve a variety of substances, each with unique effects and challenges in treatment. These substances can be legal, such as alcohol and prescription medications, or illegal, like heroin or cocaine. The different category types of drug addictions are listed below.
Alcohol Use Disorder (AUD)
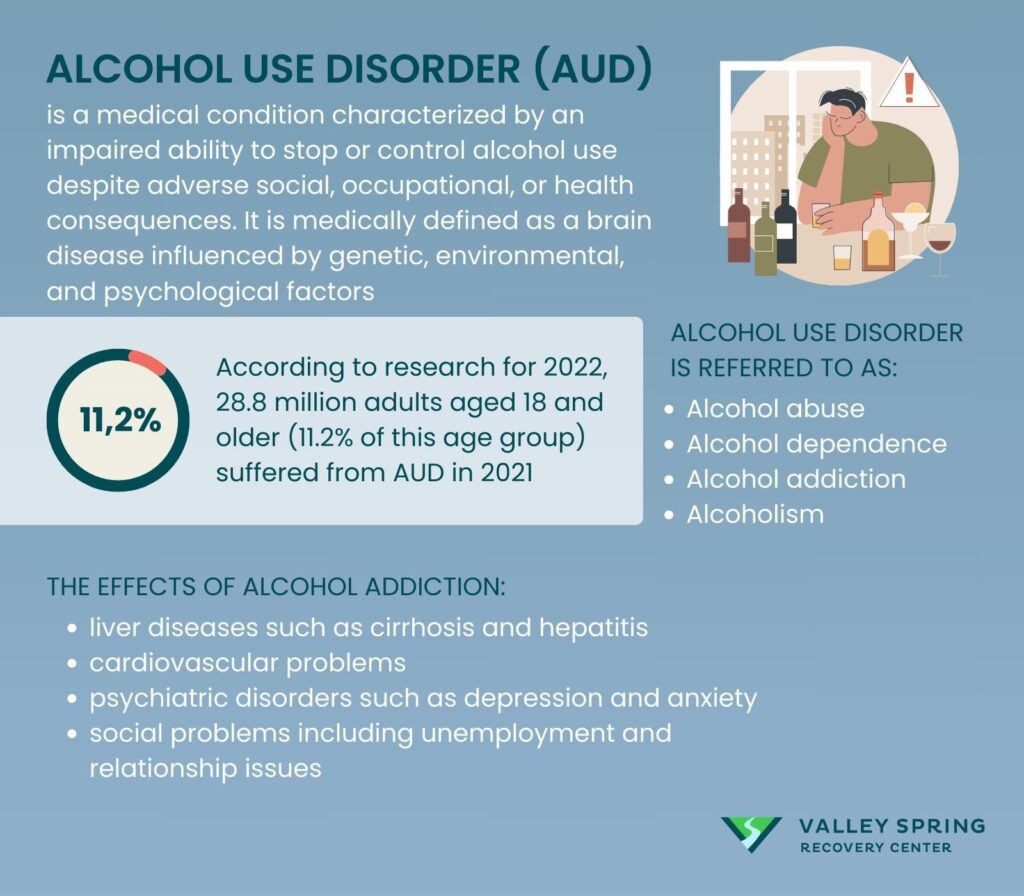
Alcohol use disorder (AUD) is a medical condition characterized by an impaired ability to stop or control alcohol use despite adverse social, occupational, or health consequences. It is medically defined as a brain disease influenced by genetic, environmental, and psychological factors that can be mild, moderate, or severe according to a 2020 report on Alcohol’s effects on health by the National Institute of Alcohol Abuse and Alcoholism (NIAAA). Alcohol Use Disorder is referred to as alcohol abuse, alcohol dependence, alcohol addiction, and alcoholism.
According to the 2022 National Survey on Drug Use and Health and the Center for Behavioral Health Statistics and Quality’s 2022 study, 28.8 million adults aged 18 and older (11.2% of this age group) suffered from AUD in 2021. An estimated 753,000 adolescents ages 12 to 17 (2.9% of this age group) had AUD during this time frame.
The effects of Alcohol Use Disorder (AUD) can lead to devastating long-term health consequences including liver diseases such as cirrhosis and hepatitis, cardiovascular problems, psychiatric disorders such as depression and anxiety, and social problems including unemployment and relationship issues. The World Health Organization 2022 fact sheet on alcohol reveals alcohol misuse is the world’s third-largest risk factor for disease and mortality, responsible for an estimated 3 million deaths globally each year, representing 5.3% of all deaths.
According to Dr Michael Olla, an addiction psychiatrist, treatment for alcohol addiction includes a combination of therapies, medication, and support groups. Detoxification under medical supervision is often the first step, followed by behavioral therapies like cognitive-behavioral therapy (CBT) and motivational enhancement therapy (MET). Medications such as naltrexone, acamprosate, and disulfiram are also used to help reduce drinking and prevent relapse. Support from organizations such as Alcoholics Anonymous (AA) offers a community-based approach to recovery, emphasizing peer support and accountability.
Tobacco and Nicotine Addiction
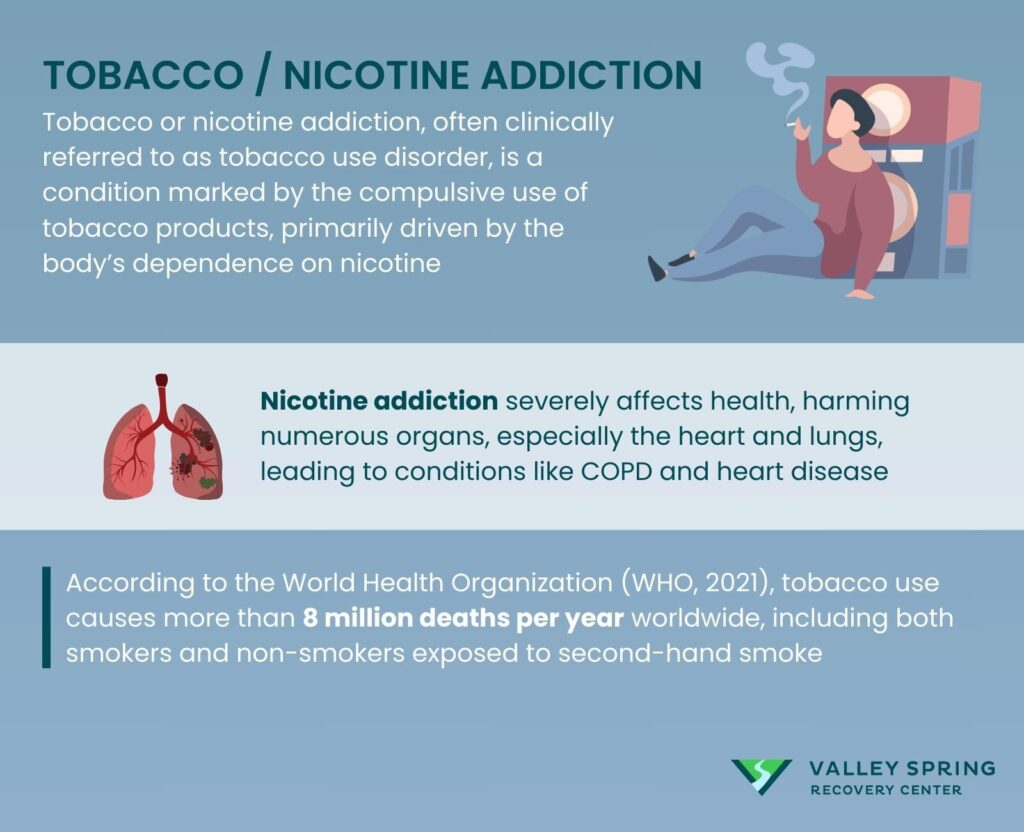
Tobacco or nicotine addiction, often clinically referred to as tobacco use disorder, is a condition marked by the compulsive use of tobacco products, primarily driven by the body’s dependence on nicotine. This chemical is highly addictive, affecting the same brain pathways as heroin and cocaine. The Centers for Disease Control and Prevention (CDC) 2020 report highlights that nicotine addiction is the most prevalent form of chemical dependence in the United States. It alters brain chemistry, making quitting smoking exceptionally challenging.
The health impacts of nicotine addiction are severe and widespread, affecting nearly every organ in the body. It is particularly detrimental to the cardiovascular and respiratory systems, leading to diseases such as chronic obstructive pulmonary disease (COPD) and heart disease. According to the World Health Organization (WHO, 2021), tobacco use causes more than 8 million deaths per year worldwide, including both smokers and non-smokers exposed to second-hand smoke. Cigarette smoking alone kills more than 480,000 Americans each year according to the U.S. Department of Health and Human Services Office on Smoking and Health 2014 research.
Addressing nicotine addiction requires a multi-pronged treatment approach that includes Nicotine Replacement Therapy (NRT) products like gums, patches, and lozenges are commonly used to mitigate withdrawal symptoms and decrease the urge to smoke. Non-nicotine medications such as bupropion and varenicline have also been effective in helping individuals quit by targeting the brain’s nicotine receptors. Furthermore, behavioral therapies and support groups provide the psychological support needed to overcome addiction. The American Lung Association 2023 Tobacco Cessation article emphasizes combining these treatments to increase the chances of successfully quitting and was reaffirmed by the U.S. Surgeon General’s Report on Smoking Cessation, released January 23.
Opioid Addiction
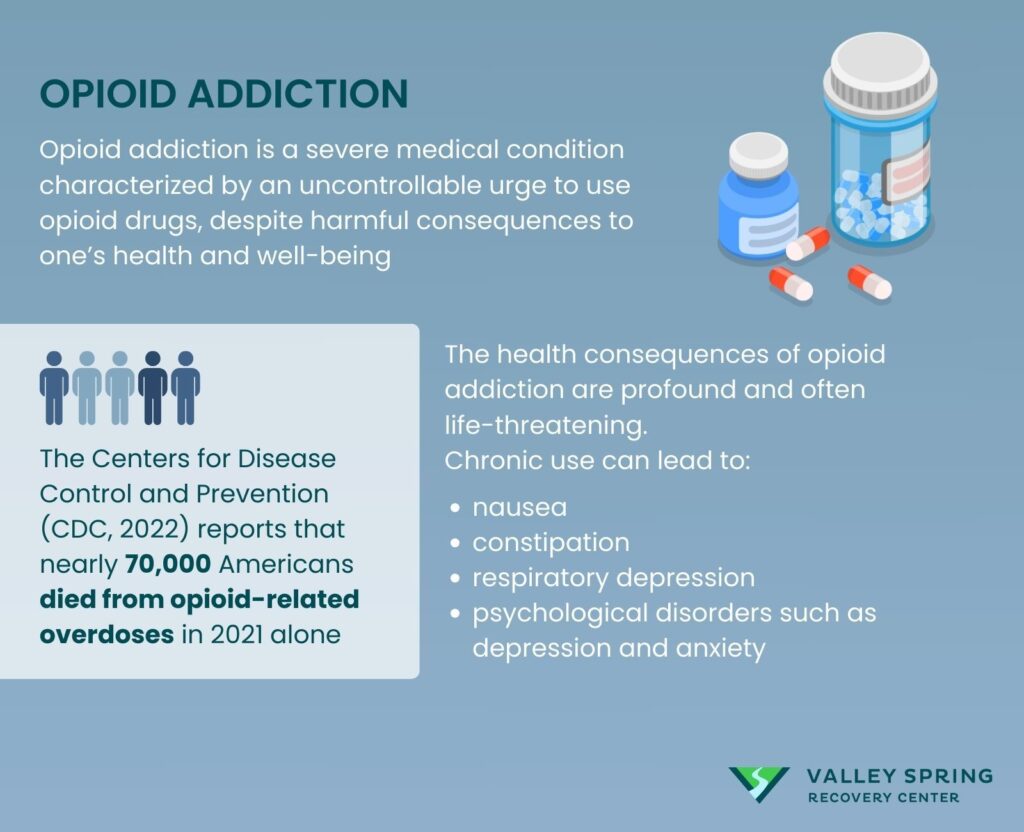
Opioid addiction is a severe medical condition characterized by an uncontrollable urge to use opioid drugs, despite harmful consequences to one’s health and well-being. Opioids, which include both illegal drugs like heroin and prescription pain relievers such as oxycodone and morphine, act on the nervous system to produce pain-relieving and euphoric effects. According to the National Institute on Drug Abuse (NIDA, 2020), opioid addiction can disrupt significant aspects of life, leading to physical and psychological dependence that requires more than willpower to overcome.
The opioid epidemic has become a public health crisis, especially in the United States. The Centers for Disease Control and Prevention (CDC, 2022) reports that nearly 70,000 Americans died from opioid-related overdoses in 2021 alone. This statistic highlights the urgent need for effective intervention strategies and broader public awareness about the dangers of opioid misuse.
The health consequences of opioid addiction are profound and often life-threatening. Chronic use can lead to nausea, constipation, respiratory depression, and psychological disorders such as depression and anxiety. Long-term use also increases the risk of infectious diseases like HIV and hepatitis due to needle sharing. The World Health Organization (WHO, 2022) emphasizes that opioid addiction not only affects the individual’s health but also has significant social and economic impacts, contributing to increased healthcare costs and productivity losses.
Treatment for opioid addiction is comprehensive and often includes both medications and behavioral counseling. Medication-assisted treatment (MAT) is considered the gold standard, using medications such as methadone, buprenorphine, and naltrexone to reduce withdrawal symptoms and cravings. These treatments are most effective when combined with behavioral therapies that address the underlying causes of addiction, according to the Substance Abuse and Mental Health Services Administration (SAMHSA, 2022). Support groups and community resources also play a crucial role in recovery, providing ongoing support to prevent relapse.
Stimulant Addiction
Stimulant addiction refers to the compulsive use of substances that increase activity in the brain and nervous system, enhancing alertness and energy. Common stimulants include prescription medications such as amphetamines (Adderall, Ritalin) and illicit drugs like cocaine and methamphetamine. As noted in the National Institute on Drug Abuse’s 2020 report, stimulants significantly affect neurotransmitters in the brain, which contributes to the high potential for addiction and abuse.
The use of stimulants can lead to severe psychological and physical health issues. Psychologically, it can cause paranoia, increased aggression, and in some cases, severe mental health disorders like psychosis. Physically, stimulants raise heart rate and blood pressure, which can lead to cardiovascular problems, including heart attacks, as mentioned in a study published by the American Heart Association in 2021. Chronic use may also result in neurological damage and a decline in physical health due to malnutrition and lack of sleep.
Treating stimulant addiction often involves a combination of pharmacological and behavioral interventions. There are currently no FDA-approved medications to treat addiction to cocaine or methamphetamine, making behavioral therapies like cognitive-behavioral therapy and contingency management crucial, as highlighted in the Substance Abuse and Mental Health Services Administration’s 2022 guidelines on behavioral health treatments. Support groups and inpatient or outpatient treatment programs also provide necessary support, as these environments help prevent relapse and address the underlying causes of addiction.
Cannabis Addiction
Cannabis addiction, often termed cannabis use disorder or marijuana use disorder, is characterized by the compulsive use of cannabis despite adverse consequences in personal, professional, or social contexts. According to the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), as referenced in a 2022 report by the National Institute on Drug Abuse (NIDA), cannabis addiction is increasingly prevalent due to higher potency strains and greater societal acceptance.
Long-term cannabis use can lead to significant health issues including respiratory problems from smoking, altered brain development in younger users, and cognitive impairments affecting memory and attention. A 2021 study by the American Psychological Association highlights that chronic users might experience mental health problems such as anxiety and depression, and in some cases, the onset of psychosis.
The treatment of marijuana addiction typically involves behavioral therapies, as there are no FDA-approved medications for its treatment. Cognitive-behavioral therapy (CBT), motivational enhancement therapy (MET), and support groups are effective in managing withdrawal symptoms and reducing cannabis use. The Substance Abuse and Mental Health Services Administration (SAMHSA, 2023) underscores the importance of tailored treatment plans that address both psychological and behavioral aspects of addiction.
Hallucinogen Addiction
Hallucinogen addiction encompasses the habitual use of substances like LSD, psilocybin, and MDMA that alter perceptions, thoughts, and emotions. These substances are not typically associated with physical dependency but can create psychological dependence. The National Institute on Drug Abuse (NIDA, 2020) reports that frequent use of hallucinogens can lead to tolerance, requiring users to consume higher doses to achieve the same effects.
The primary concern with hallucinogens is their profound impact on mental health. Users can experience intense, distressing alterations in perception, mood, and thought, known as hallucinogen-persisting perception disorder (HPPD), as per findings in the Journal of Psychopharmacology (2022). Additionally, risky behaviors during hallucinogenic experiences can lead to accidents and injuries.
Treatment for hallucinogen addiction is supportive and psychotherapeutic since there are no specific medications to counteract the effects of hallucinogens. Psychological support, such as psychotherapy and counseling, is critical in helping individuals understand and change their substance use behaviors. Group therapy can also provide peer support and decrease the stigma associated with addiction, as detailed by the American Psychiatric Association’s practice guidelines (2021).
Inhalant Addiction
Inhalant addiction involves the compulsive use of volatile substances that produce chemical vapors, which are inhaled to induce psychoactive effects. This form of addiction is particularly dangerous due to the toxic nature of the substances involved. The National Institute on Drug Abuse (NIDA, 2020) categorizes inhalants as among the most harmful substances, especially to adolescents who make up the majority of users.
Inhalants can cause immediate and severe damage to the heart, kidneys, brain, and liver. The American Medical Association (AMA, 2021) reports that sudden sniffing death syndrome is a significant risk, resulting from heart failure following abuse of inhalants. Chronic exposure can also lead to long-term cognitive deficits and neurological damage.
Treatment strategies for inhalant addiction include detoxification, medical management of withdrawal symptoms, and extensive rehabilitation programs. Because inhalant withdrawal can be particularly severe, close medical supervision is advised during detox. Behavioral interventions, including cognitive-behavioral therapy and family counseling, play essential roles in treatment plans, helping to address the root causes of addiction and promote long-term recovery, as per the guidelines from the American Society of Addiction Medicine (ASAM, 2023).
What are the most common drug addictions?
The most common drug addictions in the United States vary, with alcohol, nicotine, and marijuana topping the list due to their widespread legal status and social acceptance. Alcohol is particularly notable, with about 28.3 million people aged 12 or older reporting struggles with an alcohol use disorder as of 2020. Nicotine follows, with approximately 23.6 million Americans facing addiction, largely due to the legal status and accessibility of tobacco products. Marijuana also features prominently, with around 14.2 million Americans having a marijuana use disorder, a situation exacerbated by increasing legalization and social acceptability of the drug.
What Are The Most Expensive Illegal Drugs?
The costs of the most expensive illegal drugs vary significantly, reflecting their potency and the risks associated with their use. Cocaine is one of the most expensive, costing between $80 to $100 per gram, reflecting its high demand and the dangers involved in its trade and use. Heroin follows, with a cost of about $15 to $20 per dose, attributed to its high risk of addiction and overdose. Methamphetamine varies widely in price, from $3 to $500 per dose, depending on its form and purity.
What Are The Signs and Symptoms Of Addiction?
Addiction can be identified through the symptoms addiction causes, including various physical, emotional, psychological, and behavioral signs that impact an individual’s health, mood, and daily activities.
There are 3 categories of signs and symptoms which include:
Physical symptoms stand out as clear indicators of addiction. A hallmark of drug addiction includes noticeable neglect in appearance, with individuals appearing disheveled and displaying a disregard for personal hygiene or grooming due to prioritizing substance use above self-care. Significant health issues also emerge, spanning digestive to respiratory problems. Furthermore, weight fluctuations become evident as addiction impacts appetite and metabolism directly.
Emotional and psychological symptoms, while less visible, are equally indicative of addiction. Mood swings, marked by sudden and severe emotional shifts from euphoria to deep irritability or sadness, disrupt the life of the addict and those around them. Anxiety and depression frequently occur, characterized by persistent worry, sadness, or a sense of hopelessness. These emotional states often perpetuate the addiction cycle, with substances used as a form of self-medication, worsening the underlying issues.
Behavioral changes are critical in diagnosing addiction. Alterations in daily routines, interests, and activities serve as significant warnings. For example, a previously punctual and responsible individual could begin to miss appointments or fail to fulfill obligations causing work or academic performance to suffer as a result of the addiction. Additionally, social isolation becomes a pronounced behavior, with the individual pulling away from family, friends, and social activities, either to conceal their addiction or because substance use dominates their life.

Below are specific signs not broken down by category that indicate an addiction is present:
- Fluctuations in Appetite and Weight: Sudden weight gain or loss may be an indicator.
- Changes in Sleep Patterns: Insomnia or oversleeping can be a symptom.
- Altered Energy Levels: Sudden bursts of energy or, conversely, lethargy can be telling signs.
- Withdrawal Symptoms: Physical discomfort or illness when attempting to quit a substance.
- Stockpiling Substances: Keeping hidden stashes of the addictive substance.
- Change in Physical Appearance: Looking consistently tired, disheveled, or haggard.
- Mood Swings: Extreme emotional highs and lows.
- Inability to Stop: Despite attempts, failing to quit the substance or activity.
- Denial: Refusing to acknowledge the problem.
- Loss of Interest: Neglecting activities or hobbies once enjoyed.
- Prioritization: Putting the addictive substance or behavior above all else, including family and work.
- Secrecy and Deception: Lying or being secretive about activities, potentially even stealing to support the addiction.
- Isolation: Increasing preference for solitude, avoiding social gatherings or family events.
- Social Circle Changes: Starting to associate with a new, often enabling, group of friends.
- Financial and Legal Troubles: Accumulating debt or facing legal consequences related to the addiction.
- Engagement in Dangerous Activities: Taking unnecessary risks, possibly to obtain the substance or engage in the behavior.
- Ignoring Negative Consequences: Continuing the addictive behavior despite obvious harm or danger.
- Excessive Consumption: Using more of the substance than initially intended or medically recommended.
Understanding these nuanced symptoms can aid in early detection and intervention, thereby opening the path for more effective treatment options such as counseling, medication, and support groups tailored to the individual’s specific needs.
What Are The Causes Of Addiction?
The causes of drug addiction encompass biological determinants, environmental catalysts, psychological and emotional triggers, and developmental and behavioral factors, highlighting the complex interplay of genetics, upbringing, mental health, and early substance exposure according to the 2024 NIDA report titled “Drug Misuse and Addiction”.
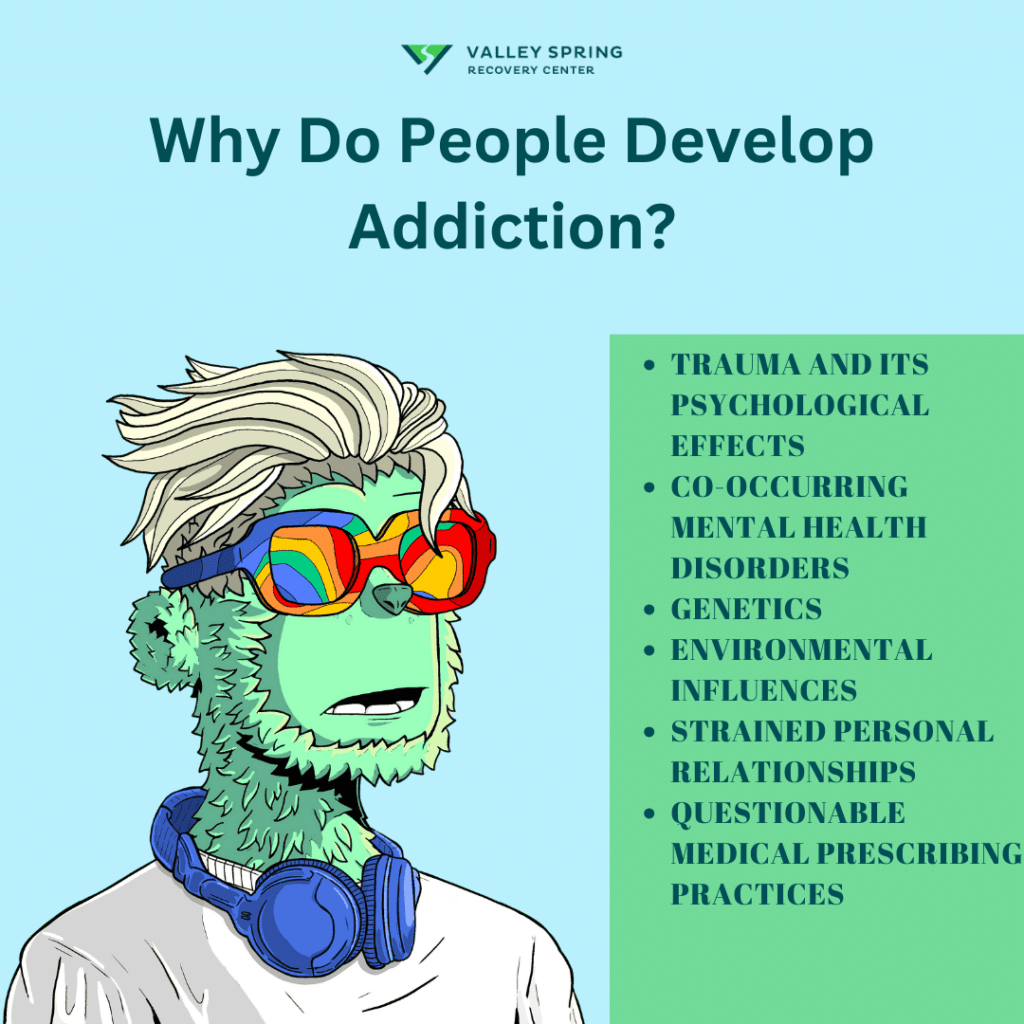
- Biological Determinants: Genetic factors significantly influence an individual’s predisposition to substance dependency. A combination of genetic variables directly impacts vulnerability to addiction. Moreover, neurodevelopmental factors, notably the ongoing development of the prefrontal cortex in adolescents, heighten the risk of substance dependency, especially with early substance exposure.
- Environmental Catalysts: The environment plays a crucial role in determining the likelihood of addiction. Peer groups that promote substance misuse often encourage similar behaviors in others. A family history of substance abuse intensifies this risk. Additionally, socioeconomic barriers, such as limited access to education and healthcare, increase susceptibility to addiction. These environmental influences are pivotal during critical developmental stages, shaping an individual’s addiction risk.
- Psychological and Emotional Triggers: Continuous stress and negative life events are significant psychological triggers for substance dependency. Disorders like Post-Traumatic Stress Disorder (PTSD), depression, and anxiety frequently accompany addiction, necessitating a dual-diagnosis approach for effective treatment. Peer pressure, along with physical and sexual abuse, early drug exposure, stress, and the role of parental guidance, profoundly influences an individual’s risk of substance use and addiction.
- Developmental and Behavioral Factors: Early initiation of substance use markedly increases the risk of developing a long-term dependency. Certain personality traits or disorders predispose individuals to addiction. A comprehensive understanding of these diverse risk factors offers a holistic perspective on susceptibility to addiction, highlighting the complex interaction between biological, environmental, and psychological factors.
Genetics predispose individuals to addiction, but environmental factors like stress, societal pressures, and accessibility often act as triggers. It’s generally a complex interplay between the two.
Why do some people develop addiction and others do not?
Addiction, much like other complex diseases, does not develop uniformly across all individuals; various factors contribute uniquely to each person’s risk profile. Understanding why some people succumb to addiction while others do not requires a deep dive into the interplay between an individual’s biological makeup, their environmental interactions, and their developmental stages. This variance in susceptibility can be explained by a mix of risk and protective factors that either predispose individuals to addiction or shield them from it.
| Category | Factor | Description | Source |
|---|---|---|---|
| Risk Factors | Aggressive behavior in childhood | Early aggressive behaviors can lead to social isolation or conflict, increasing risk-taking behaviors, including drug use. | Grant B, et al., 2001 |
| Lack of parental supervision | Children and adolescents without adequate parental supervision are at higher risk of substance abuse. | Hill KG, et al., 2005 | |
| Low peer refusal skills | Youths who cannot refuse peer pressure are more likely to experiment with drugs, potentially leading to addiction. | Guo J, et al., 2001 | |
| Drug experimentation | Early drug use is a significant risk factor for later addiction, with early exposure often leading to greater dependence. | Chassin L, et al., 2002 | |
| Availability of drugs at school | Accessibility of drugs in educational institutions increases the likelihood of student drug use. | Sher KJ, Rutledge PC, 2007 | |
| Community poverty | Residing in impoverished neighborhoods can increase exposure to drug use and related activities, raising addiction rates. | Hawkins JD, et al., 1995 | |
| Protective Factors | Self-efficacy | A strong belief in one’s own ability to control behaviors acts as a protective factor against substance abuse. | DiClemente CC, et al., 1995 |
| Parental monitoring and support | Parents who actively engage with and support their children reduce their risk of addiction by shielding them from negative influences. | Hill KG, et al., 2005 | |
| Positive relationships | Strong, healthy relationships with peers and adults provide emotional security and reduce the likelihood of drug use. | Duncan GJ, et al., 2006 | |
| Good grades | Academic success is linked to higher self-esteem and reduced engagement in risky behaviors, including drug use. | Bond L, et al., 2007 | |
| School anti-drug policies | Effective school policies and programs can deter drug use by educating students on the dangers of drug abuse and enforcing rules that discourage drug use. | Sher KJ, Rutledge PC, 2007 | |
| Neighborhood resources | Access to community resources like recreational centers and libraries provides alternatives to drug use and supports healthy lifestyles. | Chalk R, Phillips DA, 1997 |
How Does Genetics Influence Addiction?
Genetics can play a significant role in addiction. While having a family history of addiction doesn’t guarantee that one will develop an addiction, it does increase the risk. Various genes affecting neurotransmitters and their receptors have been linked to addictive behaviors, although environmental factors also play a crucial role.
What Are The Effects of Addiction?
The effects and consequences of drug addiction are far-reaching and profoundly impact nearly every part of an individual’s life, affecting their physical health, emotional well-being, relationships, and even their standing in society.
- Physical Health: One of the most immediate effects of drug addiction is physical health. Depending on the substance abused, individuals experience a range of health issues including liver damage, respiratory problems, cardiovascular diseases, stroke, cancer, and infectious diseases like HIV/AIDS from shared injection equipment.
- Mental Health: Drug addiction often co-occurs with a range of mental health issues, such as depression, anxiety, and schizophrenia. Substance abuse exacerbates mental health conditions, creating a vicious cycle that’s difficult to break.
- Relationships: Addiction strains relationships with loved ones due to erratic or violent behavior, neglect of responsibilities, and other negative consequences of drug use. This often leads to isolation from family and friends, creating a further emotional toll.
- Economic Impact: The financial burden of sustaining a drug habit leads to job loss and homelessness. The cost of purchasing the drug, coupled with reduced productivity and increased healthcare expenses, causes financial strain.
- Legal Consequences: Drug addiction leads to a host of legal problems, including arrest, incarceration, and a lifelong criminal record, which in turn affects employment prospects and social standing.
- Social Stigma: The societal perception of drug addicts is often negative, which leads to stigmatization and further isolation. This social stigmas make it more difficult for individuals to seek help and often exacerbates the emotional toll of addiction.
- Overall Quality of Life: Ultimately, drug addiction significantly lowers the users quality of life, leading to a loss of interest in activities that once brought joy, and many times leads to overdose and premature death.
The effects of drug addiction severely impacts every aspect of an individual’s life, causing extensive physical health issues, exacerbating mental health conditions, and straining personal relationships. The economic and legal repercussions add further challenges, while societal stigma can discourage seeking necessary help. These combined effects drastically reduce quality of life, trapping individuals in a debilitating cycle of addiction that is difficult to escape without holistic treatment and strong support networks. Recognizing the multifaceted impact of addiction is essential for effective intervention and recovery.
What Are the Social Consequences of Addiction?
Addiction can have far-reaching social consequences, including strained relationships, job loss, and social isolation. The stigma associated with addiction can also lead to discrimination and reduced quality of life, making it a societal issue as well as a personal one.
What are the long-term health consequences of drug addiction?
Long-term health effects range from liver damage and respiratory issues to mental health deterioration and even death. Severity varies based on the type of drug and length of addiction.
What Are The Addiction Statistics?
Addiction is a pervasive and multifaceted issue that goes beyond personal lives, extending its reach into entire communities and industries. As explored in our previous article on the effects of drugs and alcohol in the workplace, nearly 8.7 percent of full-time workers aged 18 to 64 reported having a substance use disorder (SUD) in the past year. This prevalence varies across industries, with construction witnessing as high as 16.5%, compared to 4.3% in education services. Age and gender also play significant roles in SUD rates, with younger workers and males generally experiencing higher rates. The economic impact of substance abuse in the workplace is tangible, leading to decreased productivity, increased absenteeism, and elevated healthcare costs. According to the White House drug addiction statistics, addiction is responsible for $120 billion in lost productivity and $11 billion in healthcare costs alone. Health and Human Services states he annual economic impact of substance misuse is estimated to be $249 billion for alcohol misuse and $193 billion for illicit drug use.
What Are The Risks Of Drug Overdose as a Result of Drug Abuse?
The risks of overdosing on drugs are both significant and devastating, highlighted by escalating trends and sobering statistics that underscore the persistent challenge of drug overdose in the United States. According to the National Vital Statistics System, drug overdose deaths continue to rise, with a 14% increase from 2020 to 2021, resulting in 106,699 fatalities in the latter year. The pervasive impact of opioids, especially synthetic opioids other than methadone, remains the primary catalyst for these deaths, accounting for approximately 75.4% of all drug overdose fatalities in 2021.
Key Points on Drug Overdose Risks:
- Opioid Epidemic: In 2021, opioids were involved in 80,411 deaths, with synthetic opioids being the predominant factor. This category of drugs significantly influences the high rates of overdose deaths, reflecting their potent nature and widespread misuse.
- Increasing Rates with Psychostimulants: There is also an alarming increase in overdose deaths involving psychostimulants such as methamphetamine, often compounded by the concurrent use of synthetic opioids.
- Impact of the COVID-19 Pandemic: The pandemic exacerbated the overdose crisis, contributing to a 30% spike in drug overdose deaths from 2019 to 2020. Factors such as increased stress, anxiety, and isolation have intensified substance use and the consequent risk of overdose.
- Preventability: A notable 92% of drug overdose deaths could potentially be prevented through measures like timely administration of naloxone, improved prescription practices, and vigilant monitoring of drug use.
- Demographic Vulnerabilities: The data reveals that middle-aged men are disproportionately affected, being more than twice as likely to die from a drug overdose compared to women. Among women, the highest number of overdose deaths occurs in the 44 to 54-year age group.
- Regional Variations: There have been significant regional fluctuations in overdose death rates, with marked increases in states like Washington, Oregon, Alaska, and Nevada, and decreases in North Carolina, Wisconsin, Florida, and Georgia between 2022 and 2023.
These drug overdose statistics underscore the critical need for comprehensive strategies that include both prevention and intervention measures tailored to address the multifaceted nature of drug overdose. The ongoing efforts by organizations such as the CDC and the National Institute of Drug Abuse aim to curb these rising trends through public health initiatives and research focused on reducing the impact of this severe public health issue.
What Does Drug Addiction Do To The Brain?
Drug addiction exerts a multifaceted impact on the brain’s neural architecture, fundamentally altering its reward, cognitive, and emotional circuits. Initially, substances with addictive potential hijack the brain’s reward system, flooding it with dopamine—a neurotransmitter linked to pleasure and reinforcement. It’s important to understand the science of drug addiction as it relates to the brain because the dopamine surge from ingesting drugs not only induces an intense feeling of euphoria but also reinforces the drug-taking behavior, setting the stage for a vicious cycle of addiction. Over time, the brain adapts to these dopamine spikes by reducing the responsiveness of the neural cells in the reward circuit, a phenomenon known as ‘tolerance.’ This adaptation diminishes the individual’s ability to derive pleasure from other life-affirming activities, such as social interaction, eating, or sexual activity, thereby narrowing their sources of pleasure to the drug itself. Moreover, long-term drug use extends its damaging effects to other neural circuits, impairing cognitive functions like learning, judgment, and decision-making, while also affecting emotional regulation and stress response. Despite being cognizant of these adverse outcomes, the individual often finds themselves ensnared in a self-perpetuating cycle of substance abuse, epitomizing the paradoxical and self-destructive nature of addiction.
How do drugs interact with the brain to cause addiction?
Drugs target the brain’s reward system, flooding it with dopamine. This leads to repeated use, eventually causing changes in neural circuits that result in addiction. The brain’s reward center becomes used to receiving the dopamine spike that occurs when drugs are received into the system, making it harder and harder to stop, resulting in increased dependence.

How To Treat Drug Addiction

There are multiple types of addiction, along with various treatment types and implementations. Treatment occurs in drug rehab centers that use different treatment modalities to help addicts recover from substance use disorder. Therefore, we will discuss the different types of rehab centers where treatment is implemented: of rehab centers addiction treatment options are varied and often tailored to meet the unique needs and circumstances of each individual. Here are some of the most common types of addiction treatment options to expect:
- Medical Detox: This is usually the first step in many treatment programs. Under medical supervision, substances are safely removed from the body, ensuring that the patient is physically stable before proceeding to other forms of treatment.
- Inpatient Drug Rehab: This involves residential treatment where patients stay at a facility and receive intensive care. Inpatient treatment often includes medical observation, detoxification, therapy, and other forms of support in a controlled environment.
- Partial Hospitalization Program (PHP): Also known as “day treatment,” PHP is a more intensive form of outpatient care that allows individuals to access high-level medical and therapeutic care while living at home or in a sober living environment.
- Intensive Outpatient Program (IOP): Patients who are stable enough to live at home but still require significant treatment are the best fit for IOP according to ASAM and the DSM-5. This program involves attending treatment sessions for several hours a day but allows patients to carry on with their daily activities.
- Outpatient Treatment: This flexible option is suitable for individuals who have a strong support system at home and only need therapy or counseling services. Outpatient treatment can be customized to fit around work, school, and family commitments.
- Long-term Residential Treatment: For severe addictions, long-term residential options offer extended care that can last several months or even years.
- Therapy and Counseling: This includes a range of approaches such as individual therapy, group therapy, and family therapy. Cognitive Behavioral Therapy (CBT), Dialectical Behavior Therapy (DBT), and Motivational Interviewing are often used in these sessions.
- Alternative Therapies: These can include holistic approaches like acupuncture, art therapy, equine therapy, and mindfulness meditation as complementary treatments.
- Aftercare and Alumni Programs: Crucial for long-term recovery, these programs offer ongoing support, resources, and community to help prevent relapse.
MEDICAL DETOX
The process of medical detox involves safely removing substances from the body under the watchful eye of medical professionals. This is a critical first step in addiction treatment to ensure physical stabilization, preparing the individual for further therapeutic interventions. The importance of medical detox cannot be overstated, as withdrawal symptoms can be severe and even life-threatening. It often includes pharmacotherapy and psychological help to manage withdrawal symptoms and cravings, providing a medically stable foundation for subsequent levels of care.
INPATIENT DRUG REHAB
Inpatient drug rehab provides intensive 24/7 care within a supportive environment. The benefits of this approach include structured support, a sense of community, and comprehensive care to address all aspects of addiction. Inpatient rehab integrates various therapies, and medical protocols including individual counseling, group therapy, medication management, and holistic treatments. This setting allows for constant monitoring and immediate intervention, fostering physical, mental, and emotional recovery.
OUTPATIENT TREATMENT
Outpatient treatment offers flexibility, allowing for treatment that accommodates work, school, and family commitments. It includes therapy, counseling, support groups, and often involves PHP as well. Though less intensive than inpatient care, outpatient treatment still provides essential services, including medical management, cognitive-behavioral therapy, and relapse prevention. Outpatient care facilitates a transition back to daily life while maintaining a connection to recovery support.
THERAPY AND COUNSELING
Therapy and counseling in addiction treatment are multifaceted, involving both individual sessions tailored to each patient’s unique needs and group and family sessions that foster support and understanding among peers and family members. These therapies are often integrated into all levels of care and include various psychological and behavioral techniques, such as Cognitive Behavioral Therapy (CBT), Dialectical Behavior Therapy (DBT), and family systems therapy. Counseling often plays a role in these therapeutic interventions, ensuring that medical and psychological needs are met throughout the recovery process. Therapy and counseling are vital components in building resilience, developing coping skills, and fostering lasting recovery.
How Does Medication Play A Role In Treating Addiction?
Medications play a critical role in the treatment of drug addiction, primarily used to manage withdrawal symptoms, prevent relapse, and address co-occurring mental health conditions. The use of medication is a key component in the medical management of addiction, providing necessary biochemical support to help patients stabilize physically and mentally during the early phases of recovery.
Common medications used in addiction treatment include methadone, buprenorphine, and naltrexone for opioid addiction. These medications help to reduce cravings and withdrawal symptoms, making it easier for individuals to maintain abstinence. For nicotine addiction, patches, gum, and lozenges are often employed to aid cessation efforts. Disulfiram, acamprosate, and naltrexone are typically used for treating alcohol addiction, helping to manage withdrawal symptoms and prevent relapse.
The purpose of using these medications is to normalize brain chemistry, block the euphoric effects of drugs, and alleviate physiological cravings. Additionally, they play a crucial role in treating co-occurring mental health conditions such as depression and anxiety, which often accompany addiction. By addressing these psychological aspects, medications contribute significantly to the comprehensive treatment approach, improving overall outcomes and supporting long-term recovery.
How Do Addiction-Related Jokes, Memes and Laughter Play A Role In Recovery?
Addiction-related jokes and memes can serve as a fun way to make light of addiction, reduce stigma, and create laughter and fun in sobriety. Laughing and expressing positive emotions can be powerful tool in recovery. Many different Facebook groups and Pinterest pages have gained popularity by sharing fun jokes like the Dank Recovery Memes Facebook group where recovering addicts gather and make light of their past drama as a way of moving forward in their ongoing recovery.
Where Is Addiction Treated?

Addiction treatment is a multi-faceted endeavor that can take place in various settings, each offering a unique approach to recovery. The choice of treatment setting often depends on the severity of the addiction, the substance involved, and the individual’s specific needs. Different types of treatment providers are collectively referred to as drug rehab centers. Here is a comprehensive overview of the primary locations where addiction is treated:
Inpatient Drug Rehabilitation Centers: The most conventional setting for addiction treatment is a drug rehabilitation center. These facilities offer a structured environment that provides both medical and psychological support. They often include detoxification services, individual and group therapy, medication-assisted treatment, and aftercare planning. Rehab centers that are residential or inpatient mean the individuals reside at the facility, whereas in outpatient programs allow patients to continue living offsite.
Hospital-Based Programs: Some hospitals offer specialized addiction treatment programs, particularly for cases requiring medical detoxification or co-occurring mental health conditions. These programs provide a higher level of medical supervision compared to standard rehab centers.
Mental Health Clinics: For individuals dealing with both addiction and mental health issues, specialized mental health clinics can offer dual diagnosis treatment. These facilities provide integrated care that addresses both conditions simultaneously, improving the chances of long-term recovery.
Community Health Centers: These centers offer outpatient addiction treatment services, often at a lower cost. Community health centers provide medication-assisted treatment, counseling, and referral services for more intensive treatment if needed.
Telehealth Services: With the advent of technology, online platforms now offer telehealth services for addiction treatment. These services are particularly useful for those who cannot access traditional treatment centers due to geographical or financial constraints.
Support Groups and 12-Step Programs: Organizations like Alcoholics Anonymous (AA) and Narcotics Anonymous (NA) offer peer-led support groups. While not a substitute for professional treatment, many find these groups beneficial as a supplementary form of support.
Holistic and Alternative Therapy Centers: Some individuals opt for holistic treatments like acupuncture, yoga, and herbal medicine as adjunct therapies. While the efficacy of these methods is still under study, some find them beneficial in managing withdrawal symptoms and cravings.
frequently asked questions (FAQs) about Addiction
What is the Relationship Between Addiction and Mental Health?
The relationship between addiction and mental health is intricate and multifaceted, often leading to a complex interplay between the two. Here’s an in-depth look at this relationship:
-
Co-Occurrence: Mental health disorders and addiction often co-occur. This means that individuals struggling with addiction might also have one or more mental health conditions, such as depression, anxiety, or bipolar disorder, and vice versa.
-
Shared Risk Factors: Both mental health and addiction have shared genetic, environmental, and biological risk factors. For example, genetic predisposition, trauma, and chronic stress can increase the likelihood of both mental illness and addiction.
-
Cause and Effect: In some cases, mental health disorders might contribute to addiction. A person suffering from anxiety or depression has a higher liklihood of turning to drugs or alcohol as a form of self-medication. Conversely, chronic substance abuse can lead to mental health issues, as the effects of drugs and alcohol can alter brain chemistry and exacerbate underlying mental health symptoms.
-
Impact on Treatment: The interconnection between mental health and addiction necessitates an integrated approach to treatment. Treating one condition without addressing the other can hinder recovery. Dual-diagnosis treatment centers provide comprehensive care that addresses both mental health and substance abuse disorders simultaneously.
-
Recovery Challenges: The overlapping nature of mental health and addiction can make recovery more challenging. Symptoms of mental health disorders might trigger cravings and relapse, while withdrawal from substances might worsen mental health symptoms. Ongoing support and specialized care tailored to the individual’s specific needs are crucial.
-
Prevention and Early Intervention: Understanding the link between mental health and addiction emphasizes the importance of early intervention and prevention. Addressing mental health symptoms early, providing support, education, and therapy, can reduce the risk of developing an addiction.
-
Social and Societal Factors: Stigma surrounding both mental health and addiction can create barriers to seeking help. Encouraging open dialogue, reducing stigma, and providing accessible services are essential for supporting those affected by these interconnected issues.
The relationship between addiction and mental health is complex, characterized by a two-way influence where one condition can exacerbate the other. Recognizing and addressing this relationship is vital for effective treatment, prevention, and ongoing support. Understanding the interplay between addiction and mental health underscores the need for holistic approaches that consider the entire spectrum of an individual’s well-being.
How Does Addiction Impact the Workplace?
Substance abuse in the workplace can lead to increased absenteeism, decreased productivity, and higher healthcare costs, varying across industries. Laws concerning substance abuse in the workplace vary by jurisdiction and include implementing drug-free workplace policies, conducting drug testing, and providing Employee Assistance Programs (EAPs). Employers are tasked with balancing employee privacy rights with maintaining a safe and productive work environment, and compliance with applicable laws is crucial.
How Do Family Dynamics Influence Addiction?
Family dynamics and relationships can significantly influence an individual’s susceptibility to addiction. Dysfunctional family patterns, such as neglect, abuse, or lack of communication, increase the risk. In contrast, strong family support can be a powerful aid in recovery. Family therapy is often incorporated into treatment plans, allowing family members to understand addiction better and learn how to support their loved one effectively.
What is the Role of Support Groups in Addiction Recovery?
Support groups like Alcoholics Anonymous (AA) or Narcotics Anonymous (NA) provide a sense of community, empathy, encouragement, and accountability for those in recovery. They create a non-judgmental space where individuals can share experiences and support one another. These support systems can be essential in maintaining sobriety and provide ongoing care after formal treatment has ended.
How Does Addiction Affect Pregnancy?
Addiction during pregnancy can have serious health effects on both the mother and the unborn child, including preterm birth, low birth weight, developmental problems, and neonatal abstinence syndrome. Treatment for pregnant women with addiction often requires specialized care, focusing on both the mother’s health and the child’s development, including counseling, medical supervision, and carefully managed detoxification if necessary.
What Are the Cultural and Societal Influences on Addiction?
Cultural norms, societal pressures, and stigma can shape individual and community attitudes towards addiction. These influences affect prevalence, perception, treatment, and recovery. Understanding and addressing these factors requires a holistic approach to addiction, recognizing its complexity, and considering cultural competence and sensitivity in treatment and prevention efforts.
What Are the Latest Innovations in Addiction Treatment?
The field of addiction treatment continues to evolve with innovations like personalized therapy plans based on genetic and behavioral analysis, medication-assisted treatment that reduces cravings, telemedicine for remote access to care, and holistic approaches that integrate physical, mental, and spiritual wellness. These innovations aim to provide more effective and accessible care tailored to the unique needs of each individual.
Who is Affected by Drug Addiction?
Drug addiction is a pervasive issue that impacts not only the individual struggling with the addiction but also a wide range of people connected to them. It’s a misconception that addiction solely affects the person using the substances; its repercussions are far-reaching:
-
Family Members:
- Relatives of an addict often face emotional distress, financial strain, and social stigma. The impact on children can be particularly profound, affecting their emotional and sometimes physical well-being.
-
Friends and Social Networks:
- The social circles of an addict experience strained relationships, trust issues, and emotional fatigue due to the erratic and sometimes harmful behaviors associated with addiction.
-
Workplace and Professional Relationships:
- Addiction can lead to decreased productivity, absenteeism, and strained professional relationships, impacting businesses and colleagues.
-
Healthcare System:
- The burden on healthcare services increases due to the need for medical treatment for health issues related to addiction.
-
Community and Society at Large:
- Communities deal with higher rates of crime, increased healthcare costs, and other social issues stemming from the effects of widespread substance abuse.
Understanding that drug addiction is a multifaceted issue affecting various aspects of society can lead to more empathetic and comprehensive approaches to treatment and prevention.
Sources
- Conti, A. A., & Baldacchino, A. (2023). Early-onset smoking theory of compulsivity development: a neurocognitive model for the development of compulsive tobacco smoking.
- Abdullahi, A. A., Abidemi, O. R., & Ntozini, A. (2023). Drug addiction and marital conflicts: Exploring the experiences of drug-addicted wives in Abuja, Nigeria.
- Sarker, A., Raju, F. R., Sultana, M. P., Milon, M. M. M., & Akter, S. (2023). Exploration of drug addiction prevalence among young generation of Pabna district, Bangladesh.
- Wirogioto, A. J. (2022). Cigarette Addiction as The Gateway to Drug Addiction.
Dr. Michael Olla
All author postsShare This Post