The 12 parts of the brain affected by addiction include the prefrontal cortex, nucleus accumbens, amygdala, hippocampus, ventral tegmental area (VTA), insula, basal ganglia, hypothalamus, thalamus, orbitofrontal cortex, anterior cingulate cortex, and the brainstem. These regions are involved in processes such as decision-making, reward, memory, emotion, and stress regulation, which are all integral to the development and perpetuation of addictive behaviors.
The basal ganglia are a group of subcortical structures involved in motor control, habit formation, and reward processing. They form a key component of our brain for positive motivation and pleasure. Addiction disrupts basal ganglia function, leading to the development of compulsive drug-seeking habits and the loss of behavioral flexibility.
The prefrontal cortex is responsible for impulse control and decision-making, enabling you to take thoughtful actions. Addiction impairs impulse control, thought, and logical decision-making processes.
Substance abuse causes changes in the extended amygdala, enhancing stress reactivity and promoting anxiety and negative emotional states.
Addiction affects the nucleus accumbens (NAc) through changes in neurotransmitter levels, particularly dopamine by causing an excessive release of dopamine, overwhelming the NAc. This leads to the “high” associated with substance use but also results in the brain adapting by reducing dopamine receptors and transporters, diminishing the individual’s ability to experience pleasure from everyday activities.
The cerebral cortex is involved in higher-order functions such as sensory perception, cognition, and motor control. Addiction causes impairment in cognitive functions, affecting judgment and decision-making.
The brain stem controls basic life-sustaining functions such as heart rate, breathing, and sleeping. Addictive substances such as opioids and other depressants disrupt brain stem activity, leading to life-threatening conditions such as respiratory depression during overdose.
Addiction alters the hippocampus, leading to changes in how memories are formed and recalled, especially those related to drug use and experiences. These changes make it difficult to control drug-related cues and contexts, contributing to relapse.
The thalamus acts as a relay station, directing sensory and motor signals to various parts of the brain. It also plays a role in consciousness and alertness. Addiction affects how the thalamus processes stimuli, making it difficult for individuals to ignore cues associated with substance use.
The hypothalamus regulates vital bodily functions, including stress responses, hunger, and thirst. Addiction disrupts the hypothalamus, altering stress hormone levels and affecting basic drives.
The ventral tegmental area (VTA) is a group of neurons involved in the reward circuitry and the release of dopamine. Drugs of abuse increase dopamine release in the VTA, reinforcing drug-seeking behavior and establishing addiction.
The cingulate cortex is involved in emotion formation and processing, learning, and memory. Addiction alters the function of the cingulate cortex, impairing the ability to learn from the negative consequences of substance use.
How is The Basal Ganglia Affected By Addiction?
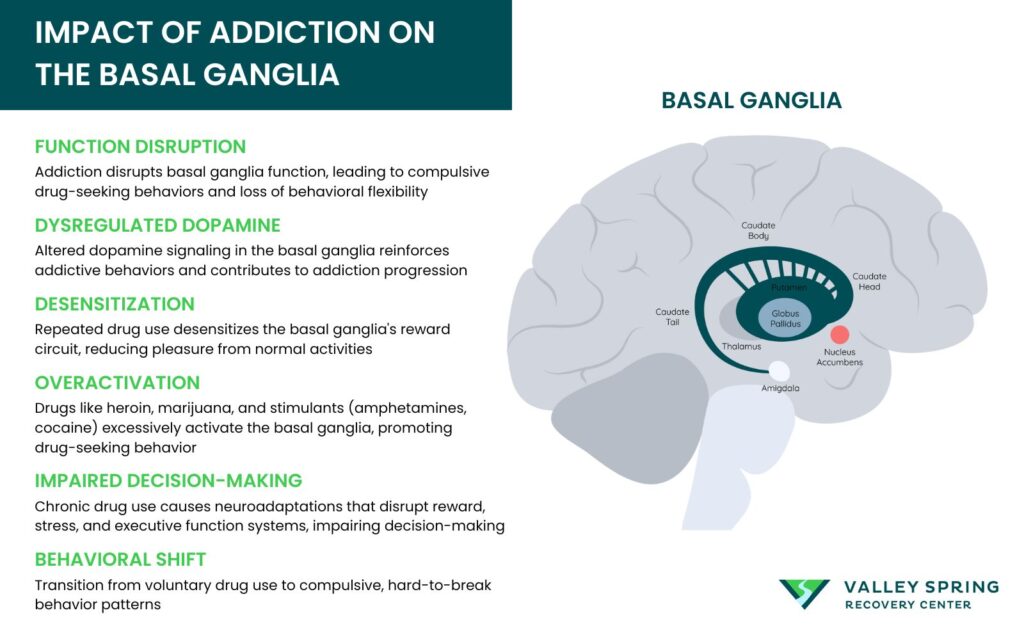
Addiction disrupts basal ganglia function, leading to the development of compulsive drug-seeking habits and the loss of behavioral flexibility.
The basal ganglia are a group of subcortical structures involved in motor control, habit formation, and reward processing. According to a 2012 study by Lanciego, J. L., et al, “Functional Neuroanatomy of the Basal Ganglia”, published in the Cold Spring Harbor Perspectives in Medicine journal, the basal ganglia has other roles including executive function and behaviors, motor learning, and emotions. In addition, this region of the brain is a key component for positive motivation and pleasure.
Addiction disrupts basal ganglia function, leading to the development of compulsive drug-seeking habits and the loss of behavioral flexibility. Dysregulated dopamine signaling in the basal ganglia reinforces addictive behaviors and contributes to the progression of addiction.
Repeated exposure to addictive substances leads to the desensitization of the basal ganglia’s reward circuit. This desensitization diminishes the ability to derive pleasure from normally rewarding activities, fostering an escalating need for the intense euphoria induced by drugs. In the cruel paradox of addiction, the relentless chase for pleasure leads to a state where pleasure becomes increasingly elusive, and previously enjoyable activities progressively get less rewarding in the absence of the substance.
Overactivation by Drugs
Drugs like heroin, marijuana, and synthetic cannabinoids imitate the brain’s natural neurotransmitters, activating neurons in the basal ganglia and paving a deceptive path to pleasure, much like impostors masquerading as musicians. Stimulant drugs such as amphetamines and cocaine exaggerate this deception by causing excessive production of neurotransmitters and prolonging the activation of the reward circuit. Electrical stimulation of the basal ganglia can also influence neuronal activation.
Excessive activation of the basal ganglia due to drug use leads to the development of drug-seeking behaviors. What begins as voluntary drug use quickly evolves into compulsive and habitual patterns.
Impaired Decision-Making
Constant activation of the basal ganglia triggers a sequence of events that disrupts the brain’s harmonious functioning. It leads to the development of drug-seeking habits, transitioning from voluntary use to a compulsive behavior pattern that is hard to break.
Chronic drug use leads to persistent neuroadaptations that impact the brain’s reward, stress, and executive function systems, impairing decision-making abilities. According to the 2015 study by Bull, P. N., et al, “Decision Making In Healthy Participants On The Iowa Gambling Task: New Insights From An Operant Approach”, the Iowa Gambling Task is used to demonstrate decision-making deficits. This decision-making deficit test is very handy in individuals dependent on substances, as they often prefer immediate rewards over long-term consequences. This distorted decision-making process serves as a stark reminder of how substance abuse disrupt the brain’s harmonious functioning, leading to enduring cognitive impairments.
What is The Effect of Addiction on Prefrontal Cortex?
Addiction affects the prefrontal cortex by disrupting inhibitory control circuits and decision-making abilities, contributing to compulsive drug-seeking behaviors. This disruption leads to impulsivity and poor judgment
The prefrontal cortex is responsible for impulse control and decision-making, enabling you to take thoughtful actions. The 2011 study by Goldstein RZ., et al, “Dysfunction Of The Prefrontal Cortex In Addiction: Neuroimaging Findings And Clinical Implications”, published in the Nature Reviews Neuroscience Journal, demonstrates that when the prefrontal cortex (PFC) is disrupted by addiction, the substance abuser is unable to control their drug intake.
Reduced Impulse Control
Substance abuse inflicts damage on the prefrontal cortex, impairing crucial abilities related to:
- Thinking
- Planning
- Decision-making
- Impulse control
Addiction also weakens the inhibitory controls of the prefrontal cortex, which is crucial for not only resisting the urge to use drugs but also indulging in risky behaviors. This loss of control escalates as individuals display impulsive behaviors like preferring smaller, immediate rewards over larger, delayed ones, indicating the severe impact of addiction on impulse control.
Cognitive Impairments
The impact of addiction on the brain is not limited to impulse control and decision-making, it also leads to cognitive impairments. Substance use including alcohol hinders spatial learning and reference memory – crucial memory processes dependent on the prefrontal cortex.
What Is The Impact of Addiction on The Extended Amygdala?
Substance abuse causes changes in the extended amygdala, enhancing stress reactivity and promoting anxiety and negative emotional states.
The extended amygdala includes structures such as the central nucleus of the amygdala (CeA), the bed nucleus of the stria terminalis (BNST), and parts of the nucleus accumbens (NAc), particularly the shell region. According to a 2016 article “ The Neurobiology Of Substance Use, Misuse, And Addiction” by the Substance Abuse and Mental Health Services Administration (SAMHSA), the extended amygdala plays a significant role in processing emotions, stress responses, and the regulation of reward-related behaviors, all of which are highly affected by addiction.
What is the Role of the Extended Amygdala in Addiction?
The extended amygdala is integral to the emotional and motivational aspects of addiction. It mediates the brain’s response to stress and anxiety, both of which are key factors in the initiation and maintenance of addictive behaviors. When an individual consumes a substance with addictive potential, such as alcohol, opioids, or stimulants, these substances trigger the release of neurotransmitters like dopamine in the brain’s reward circuits, including the extended amygdala. This release creates a pleasurable or euphoric sensation, reinforcing the behavior and promoting repeated use.
Neuroadaptations in the Extended Amygdala
According to the 2016 article from SAMHSA Chronic exposure to addictive substances leads to significant neuroadaptations within the extended amygdala. These changes include alterations in neurotransmitter systems, receptor expression, and synaptic plasticity. One key neurotransmitter involved is corticotropin-releasing factor (CRF), which plays a crucial role in the stress response. Chronic drug use increases CRF levels in the extended amygdala, enhancing stress reactivity and promoting anxiety and negative emotional states during withdrawal periods.
How Is The Nucleus Accumbens Affected By Addiction
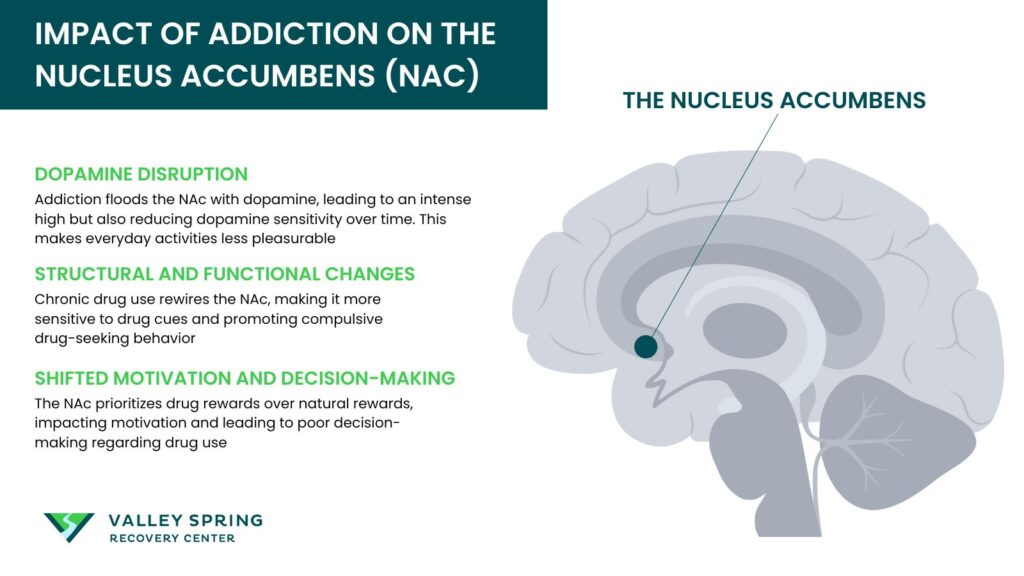
The nucleus accumbens (NAc) is a crucial brain region implicated in the reward circuitry and is significantly affected by addiction. This area, located in the basal forebrain, plays a central role in the reinforcement of rewarding behaviors, making it a key player in the development and maintenance of addictive behaviors.
Neurotransmitter Alterations
One of the primary ways addiction affects the NAc is through changes in neurotransmitter levels, particularly dopamine. In a healthy brain, dopamine is released in the NAc in response to rewarding stimuli, promoting a sense of pleasure and reinforcing behaviors. However, addictive substances, such as drugs and alcohol, cause an excessive release of dopamine, overwhelming the NAc.
According to a 2016 study by Volkow et al, “Neurobiologic Advances from the Brain Disease Model of Addiction”, this leads to the “high” associated with substance use but also results in the brain adapting by reducing dopamine receptors and transporters, diminishing the individual’s ability to experience pleasure from everyday activities.
Structural And Functional Changes
Chronic exposure to addictive substances can lead to structural and functional changes in the NAc. A 2010 study by Koob GF, et al, “ Neurocircuitry Of Addiction,” published in the Neuropsychopharmacology journal indicates that prolonged substance use alters the synaptic plasticity within the NAc, leading to persistent changes in neural circuitry. This neural remodeling contributes to compulsive drug-seeking behaviors and a heightened sensitivity to drug-related cues.
Impact On Motivation And Behavior
The alterations in the NAc due to addiction extend beyond just pleasure and reward. The region also influences motivation and decision-making. Addiction shifts the NAc’s role from processing natural rewards to prioritizing drug-related rewards. According to a 2003 study by Robinson, T. E., et al, “ Addiction”, repeated drug use sensitizes the NAc to drug-associated cues, making these cues more salient and driving compulsive drug-seeking behaviors
How Does Addiction Affect The Cerebral Cortex?
The cerebral cortex is involved in higher-order functions such as sensory perception, cognition, and motor control. Addiction causes impairments in cognitive functions, affecting judgment and decision-making.
According to a 2022 report” Drugs and the Brain”, from the National Institute on Drug Abuse (NIDA), this part of the brain is tasked with processing and interpreting sensory information, enabling thinking and reasoning, and facilitating decision-making and communication. However, when addiction occurs this cognitive harmony is disrupted, resulting in impaired cognitive function and changes in sensory perception.
The 2022 NIDA report shows that the cerebral cortex is the last part of the brain to mature. Therefore when drug use, especially marijuana, is initiated during adolescence, its development is affected leading to deficits in executive function, memory, and information processing speed. Chronic substance use is associated with alterations in brain activation patterns during the execution of cognitive tasks, suggesting an underlying neurobiological cause for the observed cognitive deficits.
Sensory Perception Changes
Drug addiction results in sensory-perceptual alterations where responses to sensory stimuli like hearing, vision, touch, smell, or kinesthetic senses can be amplified, reduced, or distorted, impacting behavior and cognitive functions. Sensory overload and sensory deprivation, conditions that can emerge from drug use, further aggravate this dissonance, potentially leading to anxiety, depression, and hallucinations.
Changes in sensory perception due to addiction cause:
- Irritability
- Restlessness
- Poor concentration
- Fluctuating mental status
What Is the Impact of Addiction on the Brain Stem?
Recreational drugs including opioids and depressants disrupt brain stem activity, leading to life-threatening conditions such as respiratory depression during overdose.
According to a 2023 study by Basinger H, et al., “ Neuroanatomy, Brainstem”, published by StatPearls, the brain stem controls basic life-sustaining functions such as heart rate, breathing, and sleeping. Addiction disrupts the brain stem’s regulation of basic life-sustaining functions like heart rate, breathing, and sleeping, triggering a cascade of harmful effects.
Disrupted Signals
Addictive substances cause neurons in the brain stem to release neurotransmitters abnormally or obstruct the normal recycling of these brain chemicals, disrupting neuron communication. Drugs and alcohol interfere with the functioning of brain cells, altering how they send, receive, and process signals throughout the body’s network.
Chronic drug use elicits a brain response that includes physical symptoms and nervous system effects like:
- Rapid heartbeat
- Paranoia
- Nausea
- Hallucinations
These symptoms occur due to disrupted signaling processes. In addition, opioid withdrawal activates the locus coeruleus-norepinephrine system, contributing to the hyperarousal and insomnia associated with withdrawal, which in turn, intensify drug cravings and relapse.
Risk of Organ Damage
The brain stem’s role in controlling vital autonomic processes is disrupted due to addiction, posing a risk of organ damage. Substance abuse compromise brain stem activity, leading to life-threatening conditions affecting heart rate and breathing.
How Does Addiction Affect The Hippocampus?
Addiction alters the hippocampus, leading to changes in how memories are formed and recalled, especially those related to drug use and experiences. These changes make it difficult to control drug-related cues and contexts, contributing to relapse.
According to a 2016 study by Kutlu, M. G., et al, “Effects Of Drugs Of Abuse On Hippocampal Plasticity And Hippocampus-Dependent Learning And Memory: Contributions To Development And Maintenance Of Addiction” the hippocampus is responsible for memory formation and spatial navigation. This part of the brain plays a crucial role in consolidating memories from short-term to long-term storage. Addictive substances disrupt this process and cause structural and functional changes in the hippocampus that underlie memory impairments.
Structural and Functional Changes
According to a 2016 study by Canales, J., “Addiction- Adult Neurogenesis in the Hippocampus”, addiction changes the hippocampus both structurally and functionally. Chronic substance use, such as alcohol and other drugs reduces the volume of the hippocampus. This size reduction is associated with impaired cognitive functions, particularly those related to memory and learning. For instance, alcohol consumption, even in moderate amounts, disrupts the formation of new memories and the recall of existing ones by interfering with the normal functioning of the hippocampus.
Neurochemical changes
The 2016 study by Canales demonstrates that addictive substances significantly change the neurochemical environment of the hippocampus. Drugs such as cocaine and opioids manipulate the release and recycling of neurotransmitters like dopamine and glutamate. These changes disrupt normal synaptic transmission and lead to the development of abnormal neural circuits associated with addiction. For instance, the euphoric effects of drugs are often linked to excessive dopamine release in the brain’s reward pathways, which includes the hippocampus. This overactivation leads to changes in how pleasure and reward are processed, reinforcing the addictive behavior
What is the Thalamus, And How is it Affected By Addiction?
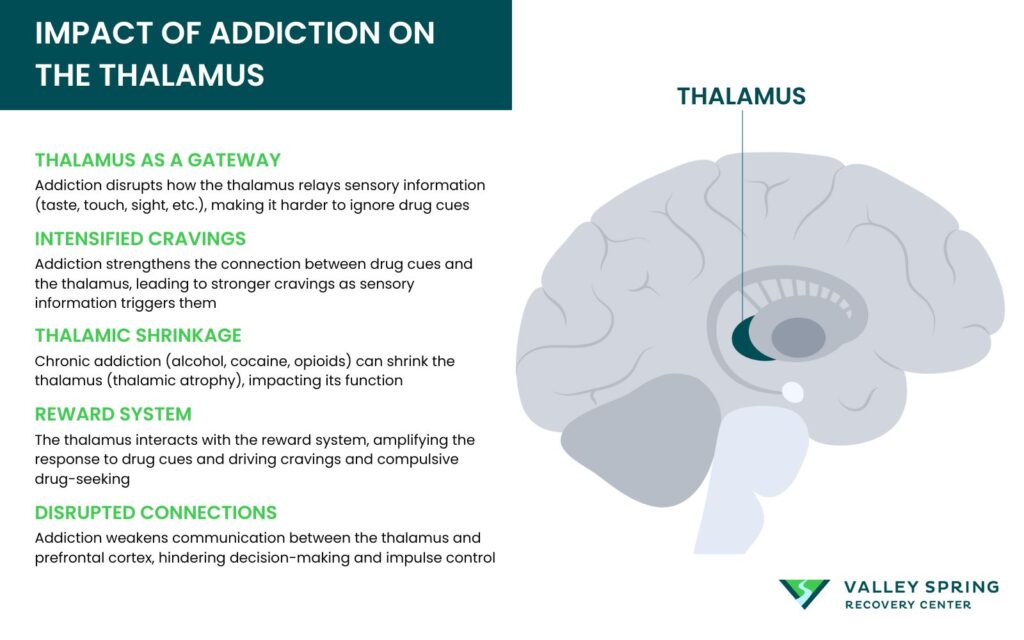
The thalamus acts as a relay station. According to the article “Thalamus Structure”, from Physiopedia, the thalamus transmits 98 percent of the sensory information to various parts of the brain. These include taste, balance, touch, and vision. It also plays a role in consciousness and alertness. Addiction affects how the thalamus processes stimuli, making it difficult for individuals to ignore cues associated with substance use.
Impairment in the thalamus due to addiction compromises the brain’s ability to selectively process stimuli, impacting how sensory information is managed and prioritized. Addiction conditions cues that provoke excessive responses from the thalamus, leading to heightened cravings as the processing of sensory information becomes skewed.
Thalamic Atrophy
A 2018 study by Huang, A. S., et al, “The Thalamus In Drug Addiction: From Rodents To Humans”, shows that addiction leads to significant changes in thalamic function and structure. Studies using imaging techniques like MRI have revealed that individuals with substance use disorders often exhibit thalamic atrophy, indicating a reduction in thalamic volume. This atrophy is associated with the chronic use of addictive substances, such as alcohol, cocaine, and opioids.
Altered Sensory Processing
The 2018 study by Huang demonstrates that the thalamus is part of the brain’s reward circuitry, and closely interacts with the prefrontal cortex and the basal ganglia. During addiction, the thalamus is involved in the heightened response to drug-related cues. This heightened response leads to increased cravings and compulsive drug-seeking behaviors, as the thalamus helps integrate sensory information with the emotional and motivational states mediated by the reward system.
In addition, addiction affects thalamic connectivity. Substance use disrupts the normal communication pathways between the thalamus and other brain regions, such as the prefrontal cortex. This disruption impairs cognitive functions, including decision-making and impulse control, which are often compromised in individuals with addiction.
What is the Hypothalamus How is it Affected by Addiction?
The hypothalamus regulates vital bodily functions, including stress responses, hunger, and thirst. Addiction disrupts the hypothalamus, altering stress hormone levels and affecting basic drives. Acute administration of addictive substances activates the hypothalamic-pituitary-adrenal axis (HPA), contributing to the initial rewarding effects and development of drug-seeking behavior.
In a 2006 study by Lovallo, W. R ., “The Hypothalamic–Pituitary–Adrenocortical Axis In Addiction”, it was demonstrated that addiction dysregulate the HPA axis, leading to altered stress hormone levels and increased vulnerability to addiction. The HPA axis activation in addiction is characterized by the release of corticotropin-releasing factor (CRF) and the subsequent release of hormones like ACTH and glucocorticoids that impact the body and brain.
Disrupted Hormone Balance
Addiction disrupts the hormonal balance in the hypothalamus. The (HPA) plays a critical role in the body’s response to stress. However, repeated drug use can lead to:
- The blunting or dysregulation of acute changes in the HPA axis
- Changes in the release of stress hormones
- Alterations in the sensitivity of receptors in the HPA axis
Dysregulation of the HPA axis during addiction is often followed by the activation of extrahypothalamic brain stress systems associated with the withdrawal/negative affect stage.
Stress System Activation
The HPA) axis, a major component of the stress system, gets activated by drugs of abuse, influencing addiction. Substances like cocaine, nicotine, and alcohol can significantly modify the stress response impacting both physiological and behavioral outcomes related to the HPA axis, and contributing to sustained addiction.
Psychostimulants like methamphetamine induce a shift in motivation towards drug use, transitioning from seeking pleasure to alleviating internal distress, implicating the acute role of the stress system in the cycle of addiction. Chronic drug use leads to sustained activation of the stress system, including hyperproduction of stress hormones and alterations in stress-related genes and proteins, which may drive withdrawal behaviors and contribute to the relapse cycle.
What Is The Ventral Tegmental Area And How is it Affected By Addiction?
The ventral tegmental area (VTA) is a part of the brain’s reward system and is involved in the release of dopamine. Addiction stimulates the VTA, leading to increased dopamine release and reinforcing the addictive behavior.
Dopaminergic Signaling and Reward
In a 2022 study, Cai, J., et al, “Anatomy and Function of Ventral Tegmental Area Glutamate Neurons” demonstrated how the VTA regulates rewards, memory, learning, and addictive behavior. The primary function of the VTA in addiction involves the release of dopamine, a neurotransmitter associated with pleasure and reward. When an individual consumes addictive substances such as opioids, cocaine, or alcohol, these substances trigger the release of dopamine from the VTA. This surge in dopamine creates feelings of euphoria and reinforces behaviors that lead to substance use. Over time, repeated exposure to addictive substances causes neuroadaptive changes in the VTA, making the brain more sensitive to these substances and driving compulsive drug-seeking behavior.
What Is The Cingulate Cortex And How It Is Affected By Addiction?
The cingulate cortex is involved in emotion formation and processing, learning, and memory. It plays a role in linking behavioral outcomes to motivation. The 2021 study by Zhao, Y., et al, “Interior Cingulate Cortex in Addiction: New Insights for Neuromodulation
Addiction” demonstrates that addiction changes the function of the cingulate cortex, impairing the ability to learn from the negative consequences of substance use.
The cingulate cortex, a crucial part of the brain’s limbic system, plays a significant role in various cognitive and emotional functions. It is subdivided into the anterior cingulate cortex (ACC) and the posterior cingulate cortex (PCC), each of which has distinct functions.
Anterior Cingulate Cortex
The ACC is involved in a range of functions, including emotional regulation, decision-making, error detection, and reward anticipation. It integrates cognitive and emotional information, allowing for appropriate responses to environmental stimuli. Dysfunction in the ACC is associated with various psychiatric disorders, including depression, anxiety, and addiction.
Posterior Cingulate Cortex
The PCC, on the other hand, is primarily associated with memory and spatial orientation. It plays a critical role in the default mode network (DMN), which is active during rest and introspection. Disruptions in the DMN have been linked to several psychiatric conditions, including addiction.
Changes in the Cingulate Cortex Due to Addiction
Anterior Cingulate Cortex (ACC)
In individuals with addiction, the ACC often shows reduced gray matter volume and altered functional connectivity. These changes are associated with impaired cognitive control, increased impulsivity, and difficulty in emotion regulation. Functional imaging studies have shown that the ACC has diminished activation during tasks requiring cognitive control and decision-making, which correlates with the severity of addiction.
- Impaired Decision-Making and Cognitive Control: Addiction leads to a shift in decision-making processes, favoring immediate rewards over long-term benefits. This is partly due to the impaired functioning of the ACC, which is critical for evaluating the consequences of actions and exerting self-control.
- Heightened Sensitivity to Drug-Related Cues: The ACC becomes hyper-responsive to drug-related stimuli, which can trigger cravings and relapse. This heightened sensitivity is due to neuroadaptive changes that enhance the salience of drug-related cues over natural rewards.
- Emotional Dysregulation: The ACC’s role in regulating emotions is compromised in addiction, leading to increased anxiety, depression, and stress. These emotional states can further drive drug-seeking behavior as individuals attempt to self-medicate negative emotions.
Posterior Cingulate Cortex (PCC)
The PCC is also affected by addiction, with alterations in both its structure and function. Functional MRI studies have shown disrupted connectivity within the DMN, which includes the PCC, in individuals with addiction. These disruptions are associated with impaired self-referential processing and increased vulnerability to relapse.
- Disrupted Default Mode Network (DMN): The PCC is a central node in the DMN, which is involved in self-reflection and internal thought processes. Addiction disrupts the connectivity within the DMN, leading to difficulties in maintaining abstinence and increased susceptibility to relapse.
- Memory and Cognitive Decline: The PCC’s involvement in memory and cognitive functions is compromised in addiction. This can result in impaired autobiographical memory and difficulties in forming new memories, which are essential for learning new coping strategies and maintaining recovery.
Cravings and Urges
In the 2021 study, Zhao showed that addiction leads to a decrease in the cingulate cortex’s ability to control cravings and urges. This makes it harder to resist substance use despite the negative consequences.
What Is The Insula And How It Is Affected By Addiction?
The insula is linked to the conscious awareness of the body and emotions. It is also involved in the craving and urge to use addictive substances. Changes in the insula significantly affect addiction, making people using substances experience cravings for them.
In a 2010 study, Garavan H., “ Insula And Drug Cravings” demonstrated that insula’s involvement in addiction is attributed to its role in processing and integrating interoceptive signals, which are the body’s internal physiological states. These signals are crucial for the subjective experience of craving. For instance, when a person addicted to nicotine experiences a craving, the insula integrates signals related to the body’s need for nicotine and the emotional response to that need.
The insula also contributes to decision-making processes under conditions of risk and uncertainty, which are often encountered in addiction. It helps mediate the conscious urges to take drugs by processing the reward-related information and the interoceptive states that signal the need for the substance
Are Addicts Narcissists?
Not all individuals with narcissism have an addiction, and vice versa. While some people with narcissism may also have addictions, it is not a universal characteristic of the condition. According to a 2001 study, by Baumeister, R. F., “Narcissism as Addiction to Esteem”, addiction and narcissism are linked. However, one condition does not automatically lead to the other.
Can Brain Changes Due To Addiction Be Reversed?
While some changes in the brain due to addiction are long-lasting, sustained abstinence and appropriate treatment usually help the brain reverse most of the alterations. According to the review “ Drugs, Brains, and Behavior: The Science of Addiction
Treatment and Recovery” from the National Institute on Drug Abuse (NIDA) the brain has an immense ability to reorganize itself, allowing for some degree of recovery and adaptation. Behavioral therapies, medications, and support systems can facilitate this recovery by promoting healthy brain function and coping strategies.
Can Relapse Be Prevented?
Relapse is preventable by putting certain measures in place. According to a 2023 study by Guenzel N., “Addiction Relapse Prevention”, it is possible to prevent relapse by dealing with early symptoms of relapse. In addition, to monitoring, therapy, medications, and skill development, medications help in preventing returning to substance use.
Does Addiction Harm Other Parts Of The Body Except The Brain?
Yes, addiction affects and harms many other parts of the body except the brain. According to the NIDA review, addicted people usually present with health conditions such as lung problems, cancer, and cardiovascular problems.
Is Addiction Harmful To Other People?
Yes. Pregnant women using illicit substances risk the baby experiencing withdrawal symptoms after birth. In addition, NIDA demonstrates that children exposed to drugs usually experience development problems.
Dr. Michael Olla
All author postsShare This Post